Cytological Features of Cerebrospinal Fluid in Guillain-Barré Syndrome and Their Diagnostic Value
-
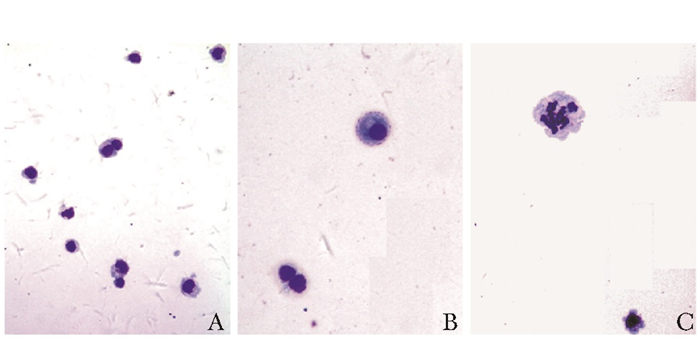
摘要:目的 探讨吉兰-巴雷综合征(Guillain-Barré syndrome, GBS)的脑脊液(cerebrospinal fluid, CSF)细胞学特点及其诊断意义。方法 回顾性分析北京协和医院2010年1月至2012年12月收治的GBS患者的临床、神经电生理和CSF检查资料。入组病例均符合《中国吉兰-巴雷综合征诊治指南》(2010年)诊断标准。CSF细胞学检查采用CSF细胞沉淀器(自然沉淀法)制片, MGG法染色。采用χ2检验比较CSF常规计数和CSF细胞学的阳性率。结果 共28例GBS患者纳入研究, 其中男19例, 女9例, 平均年龄39岁(8~69岁)。均急性起病, 肢体无力22例, 感觉减退13例, 感觉过敏3例, 球麻痹7例, 需要呼吸机辅助通气3例, 尿潴留5例, 体位性低血压1例, 眼肌麻痹5例, 面瘫10例, 共济失调4例。临床分型:急性炎性脱髓鞘性多发神经根神经病20例, 急性运动轴索性神经病1例, 急性运动感觉轴索性神经病1例, 急性感觉神经病1例, Miller Fisher综合征4例, 抗GQ1b抗体阳性的眼肌麻痹1例。CSF蛋白0.39~4.23 g/L, 蛋白升高26例, 其中11例蛋白>1.0 g/L; CSF白细胞计数:(0~5)×106/L 26例, (6~10)×106/L 2例。CSF寡克隆区带阳性者14例, 髓鞘碱性蛋白升高者18例。抗GM1抗体阳性3例, 抗GQ1b抗体阳性2例。CSF细胞学检查异常12例, 其中9例为淋巴细胞为主的炎症, 3例为单核细胞与淋巴细胞为主的炎症, 1例见2%的中性粒细胞, 6例可见激活的淋巴细胞, 2例可见激活的单核吞噬细胞, 3例可见浆细胞。病例中CSF细胞数超过5/μl者2例(7.1%), CSF细胞学提示炎性改变者12例(42.9%), CSF细胞学阳性率高于常规细胞计数(P < 0.01)。结论 GBS的CSF细胞学检查可见淋巴细胞性炎症等炎性改变, 与GBS的多发性神经根炎的病理机制相一致。与CSF常规细胞计数相比, CSF细胞学能够更敏感地显示CSF的炎性状态, 因此对于GBS也更具诊断意义。Abstract:Objective To investigate the cytological features of cerebrospinal fluid (CSF) in Guillain-Barré syndrome (GBS) and the role of the cytological features in the diagnosis of GBS.Methods We reviewed the clinical, neurophysiological, and CSF cytological findings of GBS patients treated in Peking Union Medical College Hospital from January 2010 to December 2012. The included patients all met the diagnostic criteria in 2010 China Guidelines for Diagnosis and Treatment of GBS. CSF cytological tests were performed using sedimentation chamber and MGG staining. CSF routine cell count and CSF cytological-finding positive-rate were compared with Chi-square test.Results Twenty-eight cases of GBS were included, at a mean age of 39 years (8-69 years), including 19 males and 9 females. The 28 patients all had acute onset, with 22 demonstrating limb weakness, 13 hypoesthesia, 3 hyperesthesia, 7 bulbar paralysis, 3 with the need of assisted ventilation, 5 urinary retention, 1 positional hypotension, 5 ophthalmoplegia, 10 facial paralysis, and 4 ataxia. The patients were clinically classified to acute inflammatory demyelinating polyneuropathy (20 cases), acute motor axonal neuropathy(1 case), acute motor-sensory axonal neuropathy (1 case), acute sensory neuropathy (1 case), Miller Fisher syndrome (4 cases), and GQ1b antibody-positive ophthalmoplegia (1 case). CSF protein was 0.39-4.23 g/L, increased in 26 cases, and >1.0 g/L in 11 cases. CSF white blood cell count was 0×106-5×106/L in 26 cases, and 6×106-10×106/L in 2 cases. Oligoclonal band test of CSF produced positive results in 14 cases, and myelin basic protein was found increased in 18. Anti-GM1 antibodies were positive in 3 cases and anti-GQ1b antibodies in 2 cases. Abnormal CSF cytological results were found in 12 patients, including lymphocytic inflammation in 9 and monocyte-lymphocytic inflammation in 3. The percentage of neutrophils reached 2% in 1 case. Activated lymphocytes were present in 6 cases, activated mononuclear macrophages in 2, and plasma cells in 3. The CSF cell count was over 5/μl in 2 patients (7.1%), significantly lower than the positive rate of CSF cytological test (12 cases, 42.9%, P < 0.01).Conclusions CSF cytological test in GBS could detect inflammatory changes such as lymphocyte inflammation, consistent with the pathological mechanism of polyradiculitis in GBS. Compared with CSF routine cell count, cytological test is more sensitive in revealing the inflammatory status of CSF, showing larger diagnostic value for GBS.
-
Keywords:
- Guillain-Barré syndrome /
- cerebrospinal fluid /
- cytology
-
目前, 我国每年新增肝癌患者数约占全世界新增肝癌的54%[1], 年死亡率20.4 /10万人, 占全世界肝癌死亡人数的40%。而肝脏占位的早期正确诊断是选择合适的治疗方案, 改善疾病预后的关键。临床上通过各种血清学检查、超声、CT和MRI及相关增强影像, 可使绝大多数肝脏占位能在术前明确性质, 但仍有少部分肝脏占位通过上述检查不能做出诊断, 给治疗方案的制定带来了一定的困难。本研究选取40例经全面术前检查仍不能明确诊断, 同时又有条件进行两次不同正电子发射计算机断层显像(positronemissiontomography, PET)检查的肝脏占位患者, 比较18 F-去氧葡萄糖(18 F-fluorodeoxyglucose, 18 F-FDG)和11 C-乙酸盐(11 C-Acetate)两种示踪剂PET对肝脏占位诊断的价值。
对象和方法
对象
从本科2004年10月至2010年8月经术前血清学检查, 如甲胎蛋白(α-fetoprotein, AFP)测定、B超、CT、MRI及相关增强技术仍无法明确诊断的肝脏占位患者中选取40例纳入本研究, 于术前行18 FFDG和11 C-Acetate两种示踪剂PET检查。40例患者中, 男性30例, 女性10例; 年龄31 ~ 74岁, 平均55.1岁。HBsAg(+)患者24例, HCV (+) 3例。术前肝功能分级:ChildA级37例, ChildB级3例。病例选取条件:(1)检查前均未行手术、放疗、化疗及其他治疗; (2)血清学检查、B超、CT、MRI及相关增强技术未能明确占位性质, 但临床高度怀疑恶性肿瘤; (3)全身情况、肝功能可耐受相应切除范围的手术。
方法
所有患者在行PET前均签署知情同意书, 分别在第1天和第2天空腹6 h后接受18 F-FDG-PET和11C-Acetate-PET扫描, 所用仪器为SIEMENS/CTIEXACTHR+。分别在静脉注射18 F-FDG后1 h、静脉注射11C-Acetate后10 min为扫描点, 根据肿物放射性曲线所得到的SUV值与等面积的正常肝脏组织SUV值比较, 比值≤1.0提示良性, >1.0提示恶性可能性大。
统计学处理
采用SPSS12.0统计软件, 分类变量比较采用χ2检验或配对χ2检验, 可信区间95%, P < 0.05表示差异有统计学意义。
结果
40例肝脏占位患者中39例行手术治疗, 1例经皮肝穿刺获取肿物组织。
术后病理结果
术后病理证实:40例肝脏占位患者中原发性肝细胞肝癌28例, 肝内胆管细胞癌3例, 肝血管肉瘤1例, 恶性神经内分泌肿瘤1例, 肝硬化结节伴不典型增生2例, 血管平滑肌脂肪瘤1例, 海绵状血管瘤1例, 局灶性结节性增生(FNH) 1例, 胆囊黄色肉芽肿2例。在35例恶性肿瘤和癌前病变中, 低分化7例, 中低分化5例, 中分化9例, 中高分化4例, 高分化8例, 不典型增生2例。
术前影像学及PET扫描结果
术前影像学及PET扫描结果显示:经术后病理证实的35例恶性肝脏病变和癌前病变中34例均显示病变局限于肝脏组织, 1例显示有门脉转移; 其中18F-FDG诊断恶性20例, 良性15例, 18 F-FDG对恶性病变的敏感性为57.1%, 阳性预测值为100%; 11 C-Acetate诊断恶性病变29例, 良性病变6例, 11 CAcetate对恶性病变的敏感性为82.9%, 阳性预测值为90.6%;而联合双示踪剂诊断恶性病变34例, 良性病变1例, 其对恶性病变的敏感性为97.1%, 阳性预测值为91.9%, 双示踪剂联合应用敏感性明显增加(表 1)。
表 1 肝脏占位患者正电子发射计算机断层显像结果
35例恶性肝脏病变和癌前病变中, 肿瘤最大直径 < 3 cm者18例, PET发现17例; 肿瘤最大直径≥3 cm者17例, PET发现15例, 双示踪剂PET检测小肝癌与非小肝癌发现率比较差异无统计学意义(χ2检验, χ2 =0.430, P=0.512) (表 2)。
表 2 恶性肝脏病变和癌前病变大小与正电子发射计算机断层显像结果
两种示踪剂对不同分化程度恶性肿瘤的阳性显示率不同。对于不典型增生、高分化及中高分化肝脏恶性肿瘤, 11 C-Acetate的敏感性为100%, 18F-FDG的敏感性为28.6%, 两者比较差异有显著统计学意义(配对χ2检验, χ2 =8.100, P < 0.01)。而对于低分化、中低分化肝脏恶性肿瘤, 11C-Acetate的敏感性为58.3%, 18 FFDG的敏感性为75.0%, 两者比较差异无统计学意义(配对χ2检验, χ2 =2.857, P=0.091) (表 3)。
表 3 肝脏占位病理分化程度和正电子发射计算机断层显像结果
讨论
PET是目前唯一可以了解组织分子生物学代谢改变的影像技术。通过不同的示踪剂, PET显像能体现细胞内不同分子的代谢信息, 为诊断提供依据。有报道显示PET对于原发肿瘤不明的诊断敏感性达84% ~ 93.6%[2-3], 但对肝脏原发性肿瘤诊断的报道结果并不一致, 甚至存在40% ~ 50%的假阴性率[4-7]。本研究对常规检查不能确诊的肝脏占位患者, 试图通过两种不同的PET检查以提高肝癌的术前诊断率, 并依据PET示踪剂的生物学代谢特点判断肿瘤的分化程度。
应用18 F-FDG做为PET示踪剂, 可以评价细胞内糖类的代谢。在过去的10余年中, 18 F-FDG-PET已成功地用于区分良性病变和恶性肿瘤、判定肿瘤复发、指导肿瘤分期等[6]。但在部分肝细胞肝癌中, 糖酵解并非最佳代谢途径, 其与间质组织或正常肝脏细胞类似, 因此应用PET诊断时容易出现误诊[4, 7-8]。本研究结果显示, 18 F-FDG-PET诊断肝脏恶性肿瘤的敏感性为57.1%, 阳性预测值为100%, 显示出其临床应用价值。事实上, 18 F-FDG在细胞中的代谢取决于磷酸酶和葡萄糖-6-磷酸酶的活性。在正常肝组织和分化程度好的肝细胞肝癌中, 葡萄糖-6-磷酸酶水平相对较高, FDG磷酸盐的去磷酸化相对较快, FDG在细胞内的蓄积较少[9], 因而对于分化程度好的肝癌, 18 F-FDG-PET显像与周围肝组织类似, 从而降低了其敏感性[4, 8]。本研究结果也提示, 18 F-FDG-PET检测不典型增生、高分化、中高分化肝脏恶性肿瘤的敏感性较低, 仅为28.6%;而对于低分化和中低分化肝脏恶性肿瘤, 其敏感性可高达75.0%。
11 C-Acetate作为示踪剂是近年来才开始在PET中应用的, 其首先应用于心血管、神经、泌尿系统的疾病诊断[10]。11 C-Acetate是β氧化的代谢底物, 脂肪酸和胆固醇的前体[11], 通过细胞的脂肪酸合成而进入肿瘤组织。已有文献证实11 C-Acetate-PET能用于多种恶性肿瘤的定性诊断。目前国际上应用11 C-Acetate- PET诊断肝脏肿瘤正处于起步阶段[4-5, 12-13], 在国内除本研究小组前期的报道外[14-15], 尚很少有类似报道。本研究结果显示, 11 C-Acetate-PET诊断肝脏恶性肿瘤的诊断敏感性为82.9%, 阳性预测值为90.6%, 与Ho及Park等[4, 13]报道类似, 显示出Acetate对于疑难肝脏占位的高敏感性。另一方面, 11 C-Acetate- PET对于不典型增生、高分化和中高分化肝脏恶性肿瘤的诊断敏感性为100%, 且与18 F-FDG-PET比较具有显著差异, 提示其有可能弥补18 F-FDG-PET对于中高分化程度恶性肿瘤敏感性低的劣势[8]; 而对于低分化和中低分化肝脏恶性肿瘤, 其敏感性仅为58.3%, 低于18 F-FDG-PET, 但两者比较差异无显著统计学意义, 这可能受限于病例数较少。
两种PET示踪剂的代谢方式不一样, 因此联合应用18F-FDG和11 C-Acetate进行PET扫描, 或许可以起到相互补充的作用。本研究结果显示。联合应用两种示踪剂的敏感性为97.1%, 阳性预测值为91.9%, 提高了肝脏恶性肿瘤的术前诊断率; 且两者联合应用, 有可能提示肿瘤的分化程度, 更好地指导诊断和治疗[4, 13]。
如前所述, PET检查主要取决于肿物组织内的分子代谢, 而非肿物体积。本研究应用双示踪剂PET检测, 对于小肝癌与非小肝癌的发现率无显著性差异。
综上, 对于临床上无法明确诊断的肝脏占位, PET检查虽然价格昂贵, 但仍显示了一定的优势。联合应用18 F-FDG-PET和11 C-Acetate-PET可以增加肝癌诊断的敏感性, 提高术前诊断率。根据两种示踪剂阳性不同, 可能提示恶性肿瘤的分化程度, 这对治疗方案的选择也有一定的指导意义。本研究尚需进一步累积病例, 以减少因样本量少而产生的偏倚。
-
[1] 中国吉兰-巴雷综合征诊治指南[J].中华神经科杂志, 2010, 43: 583-586. [2] Asbury AK, Arnason BG, Adams RD. The inflammatory lesion in idiopathic polyneuritis[J]. Medicine, 1969, 48:173-215. http://www.wanfangdata.com.cn/details/detail.do?_type=perio&id=WK_LWW2017052520133435
[3] 关鸿志, 王长华, 郭玉璞, 等.脑脊液细胞学的特异性发现[J].中华神经科杂志, 2004, 37:65-67. http://www.wanfangdata.com.cn/details/detail.do?_type=perio&id=zhsjk200401019 [4] Kanda T, Hayashi H, Tanabe H, et al. A fulminant case of Guillain-Barré syndrome:topographic and fibre size related analysis of demyelinating changes[J]. J Neurol Neurosurg Psychiatry, 1989, 52:857-864. DOI: 10.1136/jnnp.52.7.857
[5] Fishman RA. Cerebrospinal fluid in diseases of the nervous system[M]. Philadelphia:Saunders, 1980:175-176.
[6] 于素贞, 刘梅仕, 邓小梅, 等.多发性硬化和格林巴利综合征脑脊液细胞学及寡克隆区带测定的临床意义[J].脑与神经疾病杂志, 1994, 2:70-71. http://www.wanfangdata.com.cn/details/detail.do?_type=perio&id=QK199500836825 [7] 候熙德, 周善仁.临床脑脊液细胞学[M].南京:江苏科学技术出版社, 1985:1-120. [8] Kowarik MC, Grummel V, Wemlinger S, et al. Immune cell subtyping in the cerebrospinal fluid of patients with neurological diseases[J]. J Neurol, 2014, 261:130-143. DOI: 10.1007/s00415-013-7145-2
[9] Irani DN. Cerebrospinal fluid in clinical practice[M]. Philadelphia:Saunders, 2009:121-125.
[10] Mateen FJ, Cornblath DR, Jafari H, et al. Guillain-Barré Syndrome in India:population-based validation of the Brighton criteria[J]. Vaccine, 2011, 29:9697-9701. DOI: 10.1016/j.vaccine.2011.09.123
[11] Rauschka H, Jellinger K, Lassmann H, et al. Guillain-Barré syndrome with marked pleocytosis or a significant proportion of polymorphonuclear granulocytes in the cerebrospinal fluid:neuropathological investigation of five cases and review of differential diagnoses[J]. Eur J Neurol, 2003, 10:479-486. DOI: 10.1046/j.1468-1331.2003.00644.x
[12] 关鸿志, 陈琳, 郭玉璞, 等.脑膜淋巴瘤的临床脑脊液细胞学研究[J].中华神经科杂志, 2006, 39:114-117. http://www.wanfangdata.com.cn/details/detail.do?_type=perio&id=zhsjk200602011 [13] 关鸿志, 陈琳, 梁智勇, 等.原发中枢神经系统淋巴瘤的脑脊液细胞学诊断[J].协和医学杂志, 2012, 3:273-278. http://www.wanfangdata.com.cn/details/detail.do?_type=perio&id=xhyx201203006 [14] Machida H, Shinohara T, Hatakeyama N, et al. CD5-positive diffuse large B cell lymphoma infiltrating the central nervous system presenting Guillain-Barré-like syndrome after chemotherapy[J]. J Clin Exp Hematop, 2012, 52:199-204. DOI: 10.3960/jslrt.52.199
-
期刊类型引用(1)
1. 盛霞,秦建民. 肝脏不典型增生结节的临床特点及诊治策略. 世界华人消化杂志. 2022(04): 169-181 .  百度学术
百度学术
其他类型引用(0)

 作者投稿
作者投稿 专家审稿
专家审稿 编辑办公
编辑办公 邮件订阅
邮件订阅 RSS
RSS

 下载:
下载: