Intraoperative Intravenous Lidocaine Infusion Optimized Postoperative Pain Control and Enhanced Recovery of Gastrointestinal Function after Surgery: A Retrospective Cohort Study
-
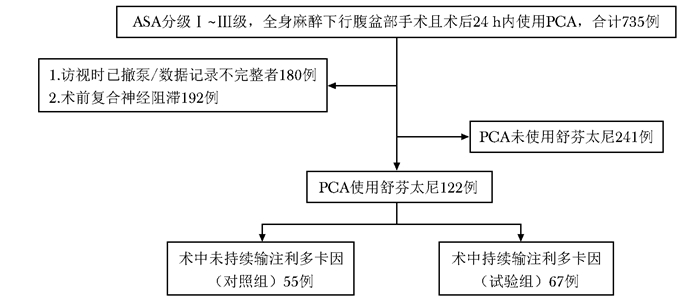
摘要:目的 观察腹盆部手术中持续静脉输注利多卡因对术后疼痛管理及胃肠道功能恢复的影响。方法 回顾性收集并分析2017年1月至2019年5月在北京协和医院接受全麻下腹盆部手术患者的临床资料, 试验组患者在全身麻醉的同时联合静脉输注利多卡因, 对照组采用传统全身麻醉模式。比较两组术后24 h内舒芬太尼的用量、静息及活动状态的疼痛视觉模拟评分(visual analogue score, VAS)、自控镇痛泵按压次数、恶心呕吐及排气情况。结果 与对照组相比, 试验组术后24 h内舒芬太尼用量和镇痛泵按压次数均减少[(0.0372±0.0137)μg/(kg·h)比(0.0498±0.0447)μg/(kg·h), t=-2.190, P=0.030;(7.4±6.7)次比(11.1±10.6)次, t=-2.257, P=0.027], 术后24 h内的静息及活动状态疼痛VAS评分≤ 3分者比例均更高(97.0%比85.5%, χ2=3.938, P=0.047;68.7%比47.3%, χ2=5.710, P=0.017), 肠道排气率更高(26.9%比5.5%, χ2=9.717, P=0.002), 但恶心、呕吐发生率未见统计学差异。结论 腹盆部手术术中输注利多卡因可能有助于术后疼痛管理, 加速胃肠道功能恢复。Abstract:Objective The aim of this study was to investigate the effect of intraoperative intravenous lidocaine infusion on pain control and the recovery of gastrointestinal function after abdominal pelvic surgery.Methods Clinical data of patients who underwent abdominal pelvic surgery under general anesthesia from January 2017 to May 2019 in Peking Union Medical College Hospital were retrospectively collected and analyzed. The patients of the control group received traditional general anesthesia, while those of the experimental group received the intravenous infusion of lidocaine based on general anesthesia. The total amount of sufentanil within the postoperative 24 h, pain visual analogue score (VAS), the number of deliveries, incidence of nausea andvomiting, the propertion of patients with intestinal passing gas were compared.Results The amount of sufentanil and the number of deliveries in the experimental group were lower than those in the control group[(0.0372±0.0137)μg/(kg·h) vs. (0.0498±0.0447)μg/(kg·h), t=-2.190, P=0.030; 7.4±6.7 vs. 11.1±10.6, t=-2.257, P=0.027]. Compared with that in the control group, the proportion of the pain VAS ≤ 3 at rest and active state in the experimental group were higher(97.0% vs. 85.5%, χ2=3.938, P=0.047; 68.7% vs. 47.3%, χ2=5.710, P=0.017), as well as the proportion of patients with intestinal passing gas(26.9% vs. 5.5%, χ2=9.717, P=0.002); there was no statistical difference in the incidence of nausea and vomiting.Conclusion Intraoperative intravenous lidocaine infusion may be helpful to optimize postoperative pain control and enhance the recovery of gastrointestinal function after surgery.
-
Keywords:
- lidocaine /
- enhanced recovery after surgery /
- multimodal analgesia
-
医学名词应使用全国科学技术名词审定委员会公布的名词。中医基础理论术语、中医临床诊疗术语、腧穴名称与部位、耳穴名称与定位均遵照相应的国家标准执行。没有通用译名的名词术语于文内第1次出现时应注明原词。中西药名以中国药典委员会编写的最新版本《中华人民共和国药典》和《中国药品通用名称》为准。确需使用商品名时应先注明其通用名称。冠以外国人名的体征、病名、试验、综合征等,人名可以用中译文,但人名后不加“氏”(单字名除外,例如福氏杆菌);也可以用外文,但人名后不加“s”。例如:Babinski征,可以写成巴宾斯基征,不写成Babinski's征,也不写成巴宾斯基氏征。已被公知公认的缩略语可以不加注释直接使用。例如:DNA、RNA、PCR等。不常用的、尚未被公知公认的缩略语,以及原词过长在文中多次出现者,若为中文可于文中第1次出现时写出全称,在圆括号内写出缩略语;若为外文可于文中第1次出现时写出中文全称,在圆括号内写出外文全称及其缩略语。例如:流行性脑脊髓膜炎(流脑),阻塞性睡眠呼吸暂停综合征(obstructive sleep apnea syndrome, OSAS)。中国地名以最新公布的行政区划名称为准;外国地名的译名以新华社公开使用的译名为准。
利益冲突 无 -
表 1 两组腹盆部手术患者一般临床资料比较
指标 对照组(n=55) 试验组(n=67) t值/χ2 P值 年龄(x±s,岁)(n=100) 49.6±15.3 52.8±14.9 -1.164 0.247 BMI(x±s,kg/m2) 22.9±3.5 23.2±3.9 -0.406 0.685 性别[n(%)] 0.058 0.810 女性 30(54.5) 38(56.7) 男性 25(45.5) 29(43.3) ASA分级[n(%)] 0.007 0.935 Ⅰ~Ⅱ级 49(89.1) 60(89.6) Ⅲ级 6(10.9) 7(10.4) 手术时间(x±s,h) 194.9±83.6 179.0±83.0 1.053 0.295 麻醉时间(x±s,h) 215.9±85.1 205.9±84.0 0.004 0.516 手术种类[n(%)] 1.818 0.178 开服 22(40.0) 35(52.2) 微创 33(60.0) 32(47.8) BMI:体质量指数,ASA:美国麻醉医师学会 表 2 两组腹盆部手术患者术后24h内舒芬太尼自控镇痛情况比较
指标 对照组(n=55) 试验组(n=67) t值 P值 舒芬太尼用量[x±s, μg/(kg·h)] 0.049 8±0.044 7 0.037 2±0.013 7 -2.190 0.030 自主按压次数(x±s, 次) 11.1±10.6 7.4±6.7 -2.257 0.027 表 3 两组腹盆部手术患者术后24 h静息及活动状态疼痛视觉模拟评分比较[n(%)]
指标 对照组(n=55) 试验组(n=67) χ2值 P值 静息状态 3.938 0.047 ≤3分 47(85.5) 65(97.0) >3分 8(14.5) 2(3.0) 活动状态 5.710 0.017 ≤3分 26(47.3) 46(68.7) >3分 29(52.7) 21(31.3) 表 4 两组腹盆部手术患者术后24h胃肠道功能恢复情况比较[n(%)][n(%)]
指标 对照组(n=55) 试验组(n=67) χ2值 P值 恶心 3.335 0.551 有 14(25.5) 14(20.9) 无 41(74.5) 53(79.1) 呕吐 0.859 0.354 有 3(5.5) 8(11.9) 无 52(94.5) 59(88.1) 排气 9.717 0.002 有 3(5.5) 18(26.9) 无 52(94.5) 49(73.1) -
[1] Palmer PP, Royal MA, Miller RD. Novel delivery systems for postoperative analgesia[J]. Best Pract Res Clin Anaesthesiol, 2014, 28:81-90. DOI: 10.1016/j.bpa.2013.12.001
[2] Minkowitz HS. A review of sufentanil and the sufentanil sublingual tablet system for acute moderate to severe pain[J]. Pain Manag, 2015, 5:237-250. DOI: 10.2217/pmt.15.22
[3] Minkowitz HS, Candiotti K. The role of sublingual sufentanil nanotabs for pain relief[J]. Expert Opin Drug Deliv, 2015, 12:845-851. DOI: 10.1517/17425247.2015.975202
[4] Meyer LA, Javier L, Iniesta MD, et al. Effect of an enhanced recovery after surgery program on opioid use and patient-reported outcomes[J]. Obstet Gynecol, 2018, 132:281-290. DOI: 10.1097/AOG.0000000000002735
[5] 王天龙, 黄宇光.推动麻醉学向围手术期医学转变:《加速康复外科中国专家共识及路径管理指南(2018版)》麻醉部分解读[J].协和医学杂志, 2018, 9:481-484. http://www.cnki.com.cn/Article/CJFDTotal-XHYX201806001.htm [6] 申乐, 黄宇光.规范化术后多模式镇痛治疗对加速腹盆部手术后康复的意义[J].中国医学科学院学报, 2016, 38:458-463. http://www.cnki.com.cn/Article/CJFDTotal-ZYKX201604016.htm [7] Feldheiser A, Aziz O, Baldini G, et al. Enhanced recovery after surgery(ERAS) for gastrointestinal surgery, part 2:consensus statement for anaesthesia practice[J]. Acta Anaesthesiol Scand, 2016, 60:289-334. DOI: 10.1111/aas.12651
[8] Nelson G, Bakkum-Gamez J, Kalogera E, et al. Guidelines for perioperative care in gynecologic/oncology:Enhanced Recovery After Surgery (ERAS) Society recommendations-2019 update[J]. Int J Gynecol Cancer, 2019, 29:651-668. DOI: 10.1136/ijgc-2019-000356
[9] 中华医学会泌尿外科学分会膀胱癌联盟加速康复外科专家协作组.根治性膀胱切除及尿流改道术加速康复外科专家共识[J].中华泌尿外科杂志, 2018, 39:481-484. [10] 耿倩, 申乐.围术期持续静脉输注利多卡因在多模式镇痛中的应用和机制探讨[J].临床药物治疗杂志, 2018, 16:80-83. http://www.cnki.com.cn/Article/CJFDTotal-LCYW201802022.htm [11] 耿倩, 李旭, 何凯, 等.多模式镇痛对妇科腹腔镜手术芬太尼用量及血流动力学的影响[J].中国疼痛医学杂志, 2017, 23:673-677. http://www.cnki.com.cn/Article/CJFDTOTAL-ZTYZ201709011.htm [12] Wal SEI, Heuvel SAS, Radema SA, et al. The in vitro mechanisms and in vivo efficacy of intravenous lidocaine on the neuroinflammatory response in acute and chronic pain[J]. Eur J Pain, 2016, 20:655-674. DOI: 10.1002/ejp.794
[13] 谭永丽, 钱金桥.静脉注射利多卡因与手术镇痛[J].云南医药, 2015, (1):87-90. http://www.cnki.com.cn/Article/CJFDTotal-YNYY201501038.htm [14] Kranke P, Jokinen J, Pace NL. Continuous intravenous perioperative lidocaine infusion for postoperative pain and recovery[J]. Cochrane Database Syst Rev, 2015, (16):CD009642. DOI: 10.1002/14651858.CD009642.pub2&doi=10.1002/14651858.CD009642.pub2&type=cdsr&contentLanguage=
[15] Dunn LK, Durieux ME. Perioperative use of intravenous lidocaine[J]. Anesthesiology, 2017, 126:729-737. DOI: 10.1097/ALN.0000000000001527
[16] Sun Y, Li T, Wang N, et al.Perioperative systemic lidoca-ine for postoperative analgesia and recovery after abdominal surgery[J]. Dis Colon Rectum, 2013, 56:271-271.
[17] Sucena M, Cachapuz I, Lombardia E, et al. Plasma concentration of lidocaine during bronchoscopy[J]. Rev Port Pneumol, 2004, 10:287-296. DOI: 10.1016/S0873-2159(15)30583-3
[18] Khan JS, Yousuf M, Victor JC, et al. An estimation for an appropriate end time for an intraoperative intravenous lidocaine infusion in bowel surgery:a comparative meta-analysis[J]. J Clin Anesth, 2016, 28:95-104. DOI: 10.1016/j.jclinane.2015.07.007
[19] 朱磊, 姜凤鸣, 金立民, 等.利多卡因静脉注射用于减轻全麻气管拔管时心血管应激反应的临床研究[J].中国实验诊断学, 2013, 17:731-732. http://www.cnki.com.cn/Article/CJFDTotal-ZSZD201304045.htm [20] Casale R, Symeonidou Z, Bartolo M. Topical treatments for localized neuropathic pain[J]. Curr Pain Headache Rep, 2017, 21:15. DOI: 10.1007/s11916-017-0615-y
[21] Baldini A, Korff MV, Lin EHB. A review of potential adverse effects of long-term opioid therapy:a practitioner's guide[J]. Prim Care Companion CNS Disord, 2012, 14.[Epub 2012 Jun 14]. doi: 10.4088/PCC.11m01326.
[22] Luca AD, Coupar IM. Insights into opioid action in the intestinal tract[J]. Pharmacol Ther, 1996, 69:103-115. DOI: 10.1016/0163-7258(95)02053-5
[23] Eleonora SG, Gollob MH, Dawood D. Voltage-gated sodium channels:biophysics, pharmacology, and related channelopathies[J]. Front Pharmacol, 2012, 3:124. https://www.researchgate.net/profile/Eleonora_Savio_Galimberti/publication/229154119_Voltage-Gated_Sodium_Channels_Biophysics_Pharmacology_and_Related_Channelopathies/links/0fcfd5106d89b15044000000/Voltage-Gated-Sodium-Channels-Biophysics-Pharmacology-and-Related-Channelopathies.pdf
[24] Beyder A, Strege PR, Bernard C, et al. Membrane permeable local anesthetics modulate NaV1.5 mechanosensitivity[J]. Channels (Austin), 2012, 6:308-316. DOI: 10.4161/chan.21202
[25] Herroeder S, Pecher S, Schönherr, et al. Systemic lidocaine shortens length of hospital stay after colorectal surgery:a double-blinded, randomized, placebo-controlled trial[J]. Ann Surg, 2007, 246:192-200. DOI: 10.1097/SLA.0b013e31805dac11
[26] Fuchs A, Rigaud M, Hogan QH. Painful nerve injury shortens the intracellular Ca2+ signal in axotomized sensory neurons of rats[J]. Anesthesiology, 2007, 107:106-116. DOI: 10.1097/01.anes.0000267538.72900.68
[27] Du C, Yu M, Volkow ND, et al. Cocaine increases the intracellular calcium concentration in brain independently of its cerebrovascular effects[J]. J Neurosci, 2006, 26:11522-11531. DOI: 10.1523/JNEUROSCI.3612-06.2006
[28] Francois A, Kerckhove N, Meleine M, et al. State-depend-ent properties of a new T-type calcium channel blocker enhance CaV3.2 selectivity and support analgesic effects[J]. Pain, 2013, 154:283-293. DOI: 10.1016/j.pain.2012.10.023

 作者投稿
作者投稿 专家审稿
专家审稿 编辑办公
编辑办公 邮件订阅
邮件订阅 RSS
RSS

 下载:
下载:











