Preoperative Medicine Treatment for Catecholamine-induced Cardiomyopathy in Patients with Pheochromocytoma/Paraganglioma
-
摘要:目的 总结嗜铬细胞瘤/副神经节瘤患者术前儿茶酚胺心肌病的药物调整方案,以期保证手术安全性。方法 回顾性收集整理2007年1月至2019年1月在北京协和医院泌尿外科接受手术治疗的嗜铬细胞瘤/副神经节瘤伴儿茶酚胺心肌病患者的临床资料,包括临床表现、超声心动图检查结果、儿茶酚胺心肌病治疗方案及治疗前后血、尿儿茶酚胺及代谢物、心功能的改变,并分析去甲肾上腺素水平与儿茶酚胺心肌病严重程度的相关性。正态分布的定量资料结果以均数±标准差表示,组间比较采用配对t检验,P<0.05为差异有统计学意义。结果 17例患者符合入选和排除标准,轻至中度心功能不全,左心室射血分数(left ventricular ejection fraction,LVEF)平均为(42.58±7.35)%,经药物治疗后所有患者心功能得到改善,LVEF较治疗前显著提高至(56.0±7.09)% (t=0.507,P=0.038)。高去甲肾上腺素组及低去甲肾上腺素组的LVEF分别为(43.11±5.79)%和(42.0±9.19)% (t=0.015,P=0.973),药物治疗后两组LVEF分别为(55.2±5.21)%和(56.87±9.07)% (t=-0.145,P=0.732),差异均无统计学意义。结论 嗜铬细胞瘤/副神经节瘤伴儿茶酚胺心肌病患者经药物治疗可有效改善心功能,去甲肾上腺素水平与儿茶酚胺心肌病严重程度无关。Abstract:Objective The aim of this study was to discuss the preoperative medicine treatment and adjustment for catecholamine-induced cardiomyopathy in patients with pheochromocytoma/paraganglioma to ensure the safety of operation.Methods The clinical information of patients with catecholamine-induced cardiomyopathy in pheochromocytoma/paraganglioma who underwent surgery in the Department of Urology at Peking Union Medical College Hospital from January 2007 to January 2019 was retrospectively collected and reviewed, including the clinical features, echocardiographic results, therapeutic strategies for catecholamine-induced cardiomyopathy, urinary catecholamine and its metabolites, and the cardiac function. The correlation between norepinephrine level and severity of catecholamine-induced cardiomyopathy was evaluated. Normal distribution quantitative data were expressed by mean±SD and analyzed by t test. The difference was statistically significant with P < 0.05.Results Seventeen patients meeting the inclusive and exclusive criteria were enrolled in this study. All patients had mild to moderate heart failure. The left ventricular ejection fraction (LVEF) before and after the medication was (42.58±7.35)% and (56.0±7.09)% respectively (t=0.507, P=0.038).The LVEF of patients with catecholamine-induced cardiomyopathy in the high norepinephrine group and low norepinephrine group were (43.11±5.79)% and (42.0±9.19)% (t=0.015, P=0.973), and after treatment, (55.2±5.21)% and (56.87±9.07)% (t=-0.145, P=0.732) respectively.Conclusions Medicine might improve the cardiac function of patients with catecholamine-induced cardiomyopathy in pheochromocytoma/paraganglioma. Norepinephrine level is not correlated with the severity of catecholamine-induced cardiomyopathy.
-
Keywords:
- pheochromocytoma /
- paraganglioma /
- catecholamine-induced cardiomyopathy /
- treatment
-
儿茶酚胺心肌病指超生理剂量儿茶酚胺释放入血后引起心肌收缩功能下降,导致心脏结构与功能异常的一类特殊心肌病。如超量儿茶酚胺由来源于交感或副交感神经系统的嗜铬细胞瘤/副神经节瘤分泌,则称为伴儿茶酚胺心肌病的嗜铬细胞瘤/副神经节瘤(catecholamine-induced cardiomyopathy in pheochromocytoma/paraganglioma,CICMPP),是嗜铬细胞瘤/副神经节瘤的一种严重并发症。儿茶酚胺可增加心肌耗氧量,诱导冠状动脉痉挛和内皮损伤从而导致微循环功能障碍,造成心肌缺血,加重心肌损伤;并通过钙超载、氧化应激、诱导凋亡、促纤维化和激活肾素-血管紧张素-醛固酮系统等作用机制直接损害心肌[1]。CICMPP常见的心脏结构与功能异常表现为对称性左心室肥大以及左心收缩功能下降,严重时引起急性左心衰,如诊疗不及时或误诊,可导致死亡。
本研究总结了北京协和医院近年接受手术治疗的CICMPP患者临床资料,探索术前调整心功能的经验和规律,以期提高手术安全性。
1. 资料与方法
1.1 研究对象
回顾性收集并分析2007年1月至2019年1月在北京协和医院泌尿外科接受手术治疗的CICMPP患者临床资料。入选标准:(1)具有包括头晕、心悸、大汗等典型嗜铬细胞瘤/副神经节瘤临床症状;(2)头、颈、躯干部有确诊为嗜铬细胞瘤/副神经节瘤的实体肿瘤,并在术后得到病理证实;(3)具备CICMPP引起心功能不全的典型临床症状,超声心动图显示左心室射血分数(left ventricular ejection fraction,LVEF)小于55%。
1.2 观察指标
分别于患者儿茶酚胺心肌病时、药物治疗后(术前)行超声心动图检查评估心脏结构及心功能变化,比较LVEF。以术前去甲肾上腺素平均水平为临界值,将患者分为高去甲肾上腺素组及低去甲肾上腺素组,并比较两组间LVEF水平差异。
1.3 儿茶酚胺心肌病的药物治疗方案
所有患者接受以下药物治疗。(1)α受体阻滞剂:常用酚苄明,口服剂量5 mg q12 h至40 mg q8 h,依据患者耐受程度给药,以不出现体位性低血压及患者耐受良好为标准;(2)β受体阻滞剂:常用倍他乐克,口服剂量12.5 mg qd至37.5 mg q12 h,心率维持在80次/min以下为宜;(3)钙离子拮抗剂:常用硝苯地平缓释片30~60 mg/d,为单用酚苄明血压控制不满意时的补充降压治疗;(4)对症治疗:针对怀疑肺部感染者加用敏感抗生素,常规扩张冠脉、强心、利尿治疗。以上治疗方案中α受体阻滞剂为必用药物,其余3种根据实际病情酌情联合使用直至术前,术后停用。
1.4 统计学处理
采用SPSS 22.0统计学软件对数据进行分析。符合正态分布的计量资料用均数±标准差,统计学分析采用配对t检验,P < 0.05为差异有统计学意义。
2. 结果
2.1 一般临床情况
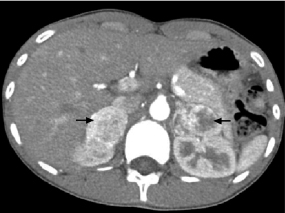
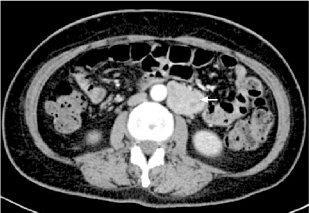
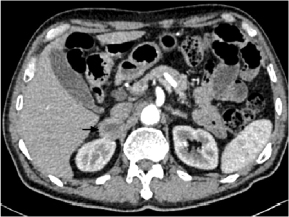
共17例符合入选标准的CICMPP患者入选本研究,其中男性8例,女性9例,年龄13~64岁,平均(32.5±10.5)岁。17例CICMPP患者中9例为单侧嗜铬细胞瘤(图 1);3例为双侧肾上腺嗜铬细胞瘤,其中2例经基因诊断为Von Hippel-Lindau综合征(图 2);此外1例为颈动脉体副节瘤,4例为腹膜后副神经节瘤(图 3)。肿瘤最大径2.6~7.2 cm,平均(4.22±0.96)cm。
17例患者均出现头痛、心悸、大汗等典型的嗜铬细胞瘤/副神经节瘤临床表现,定性定位诊断明确,24 h尿儿茶酚胺肾上腺素及去甲肾上腺素显著升高,其中肾上腺素1.75~268.75 μg/24 h,平均(26.75±9.51) μg/24 h(正常值范围:1.74~6.42 μg/24 h);去甲肾上腺素21.09~1177.27 μg/24 h,平均(565.20± 80.21) μg/24 h(正常值范围:16.69~40.65 μg/24 h),分别是正常上限的4.2倍及13.9倍。多巴胺59.51~1121.05 μg/24 h,平均(269.54±53.15)μg/24 h(正常值范围:120.93~330.59 μg/24 h),无显著升高。16例生长抑素受体(奥曲肽)显像阳性,9例肾上腺髓质全身131I-间碘苄胍(131I-metaiodobenzylguanidine,131I-MIBG)显像阳性。
2.2 药物治疗后心功能改善情况
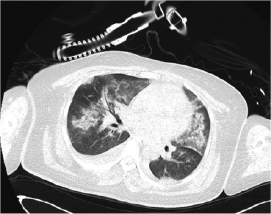
儿茶酚胺心肌病患者均有心功能不全,超声心动图提示左心室肥厚、心肌回声增强、节段性室壁运动异常。17例患者中有9例伴粉红色泡沫痰等急性左心功能不全表现,CT扫描和胸片均提示双侧肺水肿(图 4,5)。17例患者LVEF均小于55%,其中轻度异常(45%≤LVEF≤54%)者7例,中度异常(30%≤ LVEF ≤44%)者10例。17例CICMPP患者药物治疗前后的LVEF分别为(42.58±7.35)%和(56.0±7.09)%(t=0.507,P=0.038)。
2.3 尿去甲肾上腺素与左心室射血分数的相关性
以17例患者术前去甲肾上腺素平均水平565.20 μg/24 h(正常值范围:16.69~40.65 μg/24 h)为界值,将患者分为高去甲肾上腺素组(9例)及低去甲肾上腺素组(8例),两组LVEF分别为(43.11±5.79)%和(42.0±9.19)%(t=0.015,P=0.973);药物治疗后两组的LVEF分别为(55.2±5.21)%和(56.87±9.07)%(t= -0.145,P=0.732);两组药物治疗前后LVEF的差异均有统计学意义(t=0.485,P=0.045;t=0.515,P=0.037)。
2.4 手术治疗与随访
待患者血压、心率平稳,外周循环和体重增加,经超声心动图评估心脏功能好转(LVEF > 55%)后行手术治疗。17例患者肿瘤均被完整切除,其中腹腔镜切除术15例,开放手术2例(均为副神经节瘤病例),腹腔镜中转开腹手术2例。16例患者首次手术顺利,1例因首次手术麻醉时出现心律失常而暂停手术,出院后于门诊接受1个月的药物准备后再次手术。术后病理证实12例为嗜铬细胞瘤,5例为副神经节瘤。截止到2019年3月投稿时,随访3个月至12年,患者均存活,1例诊断为恶性副神经节瘤的患者于术后1年肿瘤在手术区域复发。
3. 讨论
本研究中17例患者CICMPP诊断明确,药物治疗后心功能改善,LVEF较治疗前显著提升。而去甲肾上腺素水平高低与儿茶酚胺心肌病严重程度无关。
嗜铬细胞瘤/副神经节瘤是起源于胚胎神经嵴的幅神经节细胞的神经内分泌肿瘤,位于肾上腺的称为嗜铬细胞瘤,位于肾上腺外的称为副神经节瘤,分泌儿茶酚胺,多以去甲肾上腺素为主,高儿茶酚胺血症引起高血压、心悸、大汗等临床症状。CICMPP是嗜铬细胞瘤/副神经节瘤的严重并发症,甚至可引起死亡,但往往易被忽视或误诊,因此识别并准确诊断CICMPP十分必要[2]。CICMPP的实际发生率可能高于普遍认知,据尸检报道,约50%~60%死于嗜铬细胞瘤的患者有心肌炎的典型病理改变,如局灶变性、心肌细胞收缩带坏死、炎性细胞浸润,后期以纤维化更为突出[3]。部分嗜铬细胞瘤/副神经节瘤患者虽然超声心动图检查正常,但普遍存在亚临床左心室收缩功能异常改变,并与术中出现循环衰竭的风险相关[4]。
对称性左心室肥大和左心收缩功能下降是CICMPP常见的心脏结构与功能异常,严重时出现急性左心功能不全,还可表现为扩张型[5]、肥厚梗阻型[6]、Tako-tsubo型[7]、反Tako-tsubo型、弥漫性或与冠状动脉分布不一致的节段性室壁运动障碍等[8]。本组17例患者LVEF均小于55%,存在轻中度心功能异常,9例患者伴粉红色泡沫痰等急性左心功能不全的表现。此类左心功能障碍多可逆,积极药物治疗后左心功能可部分恢复。本组患者接受药物治疗后,LVEF显著改善,提示适宜的CICMPP治疗方案有助于心功能逐步恢复。高儿茶酚胺激活心肌β2肾上腺素受体后,细胞内信号传导通路中Gs转换为Gi,导致该部位心肌产生负性肌力作用[9],推测术后心功能恢复的原因主要是由于β2-肾上腺素受体细胞内传导通路中的Gi对心肌具有保护和抗凋亡的作用[10]。
嗜铬细胞瘤/副神经节瘤手术前药物准备主要选择α受体阻滞剂,可改善外周微循环,间接扩充血容量,预先填充降压药物使用后扩大的血管床,减轻术中血压波动,避免短时间内大量补液造成心肺负荷过重引起的心血管意外发生[11]。有研究显示,使用选择性和非选择性α受体阻滞剂的患者术中整体血流动力学无显著差异[12]。
手术麻醉阶段气管插管操作本身和诱导时使用的阿片类镇静药、多巴胺受体拮抗剂类止吐药、增加交感张力的肌松药、拟交感胺类血管活性物质均可诱发儿茶酚胺大量释放[13]。本研究中1例62岁男性患者,左侧嗜铬细胞瘤,直径5.0 cm,药物治疗40 d,方案为酚苄明70 mg/d+倍他乐克12.5 mg q12 h,充分评估准备后,行手术治疗,麻醉过程中气管插管后依然出现心率失常,遂停止手术,再次给予1个月的药物调整,后顺利完成腹腔镜肿瘤切除术。该病例提示CICMPP行充分药物准备后再行手术治疗的必要性。
CICMPP的严重程度与内分泌指标并不相关。既往研究报道15例嗜铬细胞瘤患者,6例(30%,6/15)表现为左心室肥大,但血浆去甲肾上腺素或肾上腺素水平与左心室结构的测量值不相关[14]。嗜铬细胞瘤和2型糖尿病血糖变化之间的关系研究也未显示肿瘤大小及儿茶酚胺水平与血糖之间的相关性,这可能与血儿茶酚胺水平波动较大有关[15]。本组17例患者中,24 h尿去甲肾上腺素水平升高程度与LVEF下降之间无明显相关,可能是由于嗜铬细胞瘤/副神经节瘤的分泌功能呈阵发性发作,24 h尿儿茶酚胺检测仅为定性检测,无法提示肿瘤真实内分泌功能状态的差异,且分泌功能强弱与是否引发儿茶酚胺心肌病之间也无明显关联[16],儿茶酚胺心肌病的易感因素仍需进一步研究。
需要特别注意的是,本组17例中有3例为双侧肾上腺嗜铬细胞瘤,因为嗜铬细胞瘤累及双侧肾上腺,如不采用保留肾上腺功能的嗜铬细胞瘤切除术,将无法避免出现术后肾上腺皮质功能低减及长期激素替代治疗,甚至诱发Addison危象。保留肾上腺功能的双侧嗜铬细胞瘤切除术目的是保留足够的肾上腺皮质组织,避免糖皮质激素替代疗法[17]。有文献报道,采用腹膜或腹膜后路径的微创手术可使超过50%的患者保留正常皮质激素分泌功能[18],而腹腔镜手术是目前公认的治疗手段[19-20]。本研究中3例双侧肾上腺嗜铬细胞瘤患者均接受腹腔镜双侧嗜铬细胞瘤切除术,入路为后腹腔途径,先侧卧位切除一侧肿瘤,再翻身行对侧肿瘤切除术,成功保留正常肾上腺组织,避免了术后激素替代治疗,治疗效果理想。
综上所述,CICMPP是嗜铬细胞瘤/副神经节瘤的严重并发症,CICMPP患者经药物治疗可有效改善心功能,去甲肾上腺素水平与儿茶酚胺心肌病严重程度无关。
利益冲突 无 -
[1] Otusanya O, Goraya H, Lyer P, et al. A vicious cycle of acute catecholamine cardiomyopathy and circulatory collapse secondary to pheochromocytoma [J]. Oxf Med Case Reports, 2015, 10: 343-345. http://europepmc.org/articles/PMC4622181
[2] 丁莉, 方理刚, 朱文玲.嗜铬细胞瘤的心血管表现[J].中华心血管杂志, 2013, 18: 136-138. [3] Miura M, Kawano H, Yoshida T, et al. The histological features of a myocardial biopsy specimen in a patient in the acute phase of reversible catecholamine-induced cardiomyopathy due to pheochromocytoma [J]. Intern Med, 2017, 56: 665-671. DOI: 10.2169/internalmedicine.56.7454
[4] Meune C, Bertherat J, Dousset B, et al. Reduced myocardial contractility assessed by tissue Doppler echocardiography is associated with increased risk during adrenal surgery of patients with increased risk during adrenal surgery of patients with pheochromocytoma: report of a preliminary study [J]. J Am Soc Echocardiogr, 2006, 19: 1466-1470. DOI: 10.1016/j.echo.2006.06.014
[5] Park M, Hryniewicz K, Setaro JF. Pheochromocytoma presenting with myocardial infarction, cardiomyopathy, renal failure, pulmonary hemorrhage, and cyclic hypotension: case report and review of unusual presentations of pheochromocytoma [J]. J Clin Hypertens, 2009, 11: 74-80. DOI: 10.1111/j.1751-7176.2009.00073.x
[6] Jategaonkar SR, Butz T, Burchert W, et al. Echocardiac features simulating hypertrophic obstructive cardiomyopathy in a patient with pheochromocytoma [J]. Clin Res Cardiol, 2009, 98: 195-198. http://www.ncbi.nlm.nih.gov/pubmed/19205779
[7] Tanriver Y, Betz MJ, Nibbe L, et al. Sepsis and cardiomyopathy as rare clinical manifestations of pheochromocytoma: two case report studies [J]. Exp Clin Endocrinol Diabetes, 2010, 118: 747-753. DOI: 10.1055/s-0030-1253413
[8] 连鹏鹄, 丁莉, 张学斌, 等.嗜铬细胞瘤伴严重儿茶酚胺心肌病5例围手术期治疗[J].北京大学学报(医学版), 2013, 45: 605-608. DOI: 10.3969/j.issn.1671-167X.2013.04.022 [9] Paur H, Wright PT, Sikkel MB, et al. High levels of circulating epinephrine trigger apical cardiodepression in a β2-adrenergic receptor/Gi-dependent manner: a new model of Takotsubo cardiomyopathy [J]. Circulation, 2012, 126: 697-706. DOI: 10.1161/CIRCULATIONAHA.112.111591
[10] Tong H, Bernstein D, Murphy E, et al. The roles of beta-adrenergic receptor singaling in cardioprotection [J]. FASEB J, 2005, 19: 983-995. DOI: 10.1096/fj.04-3067fje
[11] 李汉忠, 张玉石.嗜铬细胞瘤/副神经节瘤的围手术期处理[J].现代泌尿外科杂志, 2012, 17: 329-332. DOI: 10.3969/j.issn.1009-8291.2012.04.002 [12] Randle EW, Balentine CJ, Pitt SC, et al. Selective versus non-selective alpha-blockade prior to laparoscopic adrenalectomy for pheochromocytoma [J]. Ann Surg Oncol, 2017, 24: 244-250. DOI: 10.1245/s10434-016-5514-7
[13] Mannelli M, Dralle H, Lenders JW. Perioperative management of pheochromocytoma/paraganglioma: is there a state of the art? [J]. Horm Metab Res, 2012, 44: 373-378. DOI: 10.1055/s-0032-1306275
[14] Galetta F, Franzoni F, Bernini G, et al. Cardiovascular complications in patients with pheochromocytoma: a mini-review [J]. Biomed Pharmacother, 2010, 64: 505-509. DOI: 10.1016/j.biopha.2009.09.014
[15] 刘志欢, 周亮, 刘志洪, 等.嗜铬细胞瘤并发2型糖尿病术后血糖变化及其预测因素[J].协和医学杂志, 2018, 9: 342-345. DOI: 10.3969/j.issn.1674-9081.2018.04.010 [16] 樊华, 李汉忠, 纪志刚, 等.伴儿茶酚胺心肌病的嗜铬细胞瘤/副神经节瘤的围手术期处理经验[J].中华泌尿外科杂志, 2018, 39: 333-337. DOI: 10.3760/cma.j.issn.1000-6702.2018.05.004 [17] 樊华, 张玉石, 李汉忠, 等.保留肾上腺功能的腹腔镜双侧嗜铬细胞瘤切除术[J].中华内分泌外科杂志, 2017, 11: 177-180. DOI: 10.3760/cma.j.issn.1674-6090.2017.03.001 [18] Castinetti F, Taieb D, Henry JF, et al. Management of endocrine disease: outcome of adrenal sparing surgery in heritable pheochromocytoma [J]. Eur J Endocrinol, 2016, 174: R9-R18. DOI: 10.1530/EJE-15-0549
[19] Sackett W, Chris P. Bilateral subtotal laparoscopic adrenalectomy for pheochromocytoma [J]. ANZ J Surg, 2003, 73: 664-666. DOI: 10.1046/j.1445-2197.2003.02699.x
[20] Wang DS, Terashi T. Laparoscopic adrenalectomy [J]. Urol Clin N Am, 2008, 35: 351-363. DOI: 10.1016/j.ucl.2008.05.009
-
期刊类型引用(2)
1. 隋莹莹,赵薇,王峥. 1例嗜铬细胞瘤伴儿茶酚胺心肌病患者围手术期的护理. 医药前沿. 2025(09): 107-110 .  百度学术
百度学术
2. 唐维晞,邓和平,陈彦汝,叶莎,张念. 心肌酶谱、动态心电图及冠状动脉CT血管造影诊断嗜铬细胞瘤儿茶酚胺性心脏损害价值研究. 现代生物医学进展. 2021(07): 1296-1300+1364 .  百度学术
百度学术
其他类型引用(0)

 作者投稿
作者投稿 专家审稿
专家审稿 编辑办公
编辑办公 邮件订阅
邮件订阅 RSS
RSS

 下载:
下载: