-
摘要:目的 分析北京协和医院神经外科纳入KC19组的垂体手术患者住院费用影响因素,为细化疾病诊断相关分组(diagnosis related groups,DRG)提供参考。方法 回顾性分析2017年1月1日至2021年11月30日北京协和医院神经外科垂体手术患者的病案首页信息,采用描述性统计、单因素分析、多因素线性回归分析患者住院费用相关影响因素。结果 本研究共纳入垂体手术患者3809例,平均住院费用为36 166.82元,平均住院天数为9.42 d;应用神经内镜手术的患者占比35.2%,存在严重并发症或合并症(major complication or comorbidity,MCC)/并发症或合并症(complication or comorbidity,CC)的患者占比40%;单因素分析发现住院费用与患者性别、住院天数、其他诊断数量、手术操作数量、是否应用神经内镜及是否存在MCC/CC有关;多因素分析发现住院费用的主要影响因素为住院时长,其次分别为其他诊断数量、手术操作数量、是否应用神经内镜、是否存在MCC/CC及性别。结论 在DRG支付方式下,KC19组的细化应着重考虑其影响因素,患者是否应用神经内镜及是否存在MCC/CC应纳入分组标准。Abstract:Objective To analyze the influencing factors of hospitalization expenses of patients treated in the KC19 group by the neurosurgery department of a tertiary hospital in Beijing, and provide reference for the refinement of diagnosis related groups(DRG).Methods The medical records of 3809 patients from January 1, 2017 to November 30, 2021 were reviewed, and relevant influencing factors were determined using descriptive statistics, univariate analysis, and multivariate linear regression.Results Among the 3809 patients included in this study, the average total hospitalization cost was 36 166.82 yuan, and the average hospital stay was 9.42 days. Neuroendoscopy accounted for 35.2%, while major complications or comorbidities (MCC) and complications or comorbidity (CC) accounted for 40%. Univariate analysis found that hospitalization costs were associated with gender, length of hospital stay, number of other diagnoses, number of surgical procedures, use of neuroendoscopy, and the presence of MCC or CC. Multivariate analysis found that the main influencing factors were the length of hospital stay, followed by the number of other diagnoses, the number of surgical operations, whether neuroendoscopy was used, whether there was MCC or CC, and gender.Conclusion In the follow-up fine grouping of KC19, the above influencing factors should be considered, and the use of neuroendoscopy and the presence of MCC or CC should be included in the grouping criteria.
-
Keywords:
- diagnosis related groups /
- hospital costs /
- pituitary tumor
-
疾病诊断相关分组(diagnosis related groups,DRG)作为在世界各地被广泛应用的临床分组方法,其重要意义在于DRG实施的预付费制度,也是我国医疗保险制度改革的重点方向。经过多年的实践探索,国家医疗保障局办公室于2019年10月发布了《国家医疗保障DRG分组与付费技术规范》和《国家医疗保障DRG(CHS-DRG)分组方案》[1],其分组理念涵盖主要诊断、手术和操作、是否存在并发症及年龄等,而DRG的试运行在为医院管理者提供预算、配置、管理工具的同时,也对临床一线工作者的决策产生重要影响,通过对DRG分组的精细化、合理化进行探索,可更大限度地发挥DRG制度的优势,使之更适合我国国情。
目前,垂体肿瘤(如泌乳素瘤和非分泌性垂体腺瘤等)的发病率正逐年升高,年发病率约为(3.9~ 4)/10万[2]。根据北京协和医院医院信息管理系统(Hospital Information System,HIS)的数据统计,2017年1月1日至2021年11月30日被分入垂体手术组(DRG分组编号为KC19)的患者数量占神经外科收治患者总数的36.6%,是神经外科DRG分组中病例占比最大的分组。虽然大部分垂体腺瘤为良性病变,但其治疗费用较高,给患者带来的经济负担不容忽视。我国的DRG按照主要诊断大类(major diagnostic category,MDC)、核心疾病诊断分组(adjacent diagnosis related group,ADRG)和DRG三层结构分类,而KC19组作为DRG分组的一个分支[3],并未考虑上级ADRG分组(KC1组)的各种复杂情况,如患者是否存在严重并发症或合并症(major complication or comorbidity,MCC)/并发症或合并症(complication or comorbidity,CC)。即使同一种疾病,在不同地区的治疗费用也存在较大差异[4]。为探寻适合我国国情的垂体手术DRG分组方法,分析KC19组内各种复杂情况是否对患者住院费用产生影响显得尤为重要。本研究通过分析北京协和医院神经外科DRG分组为KC19组的垂体手术患者数据信息,探索患者住院费用的影响因素,为DRG分组的细化及其他疾病的医保支付分析提供数据支持和参考。
1. 资料与方法
1.1 临床资料
回顾性分析2017年1月1日至2021年11月30日北京协和医院神经外科纳入KC19组的垂体手术患者病历信息,包括性别、年龄、诊断数量、主要手术操作、DRG分组、住院天数、住院费用等。
1.2 研究方法
查阅、收集2017年1月1日至2021年11月30日北京协和医院HIS系统记录在案的神经外科所有住院患者病案首页信息,按照DRG标准[3]对患者进行分类筛选,将DRG分组编号为KC19的患者信息录入Excel数据库,包括性别、年龄、诊断、主要手术操作、住院天数、住院费用等,并统计每位患者的诊断数量、主要手术操作数量,是否存在MCC/CC,按照DRG细分方案中MCC/CC标准与患者的诊断数据进行比对分析,探寻KC19组垂体手术患者住院费用相关影响因素及其对住院费用的影响程度。
1.3 统计学处理
建立Excel数据库,对患者的基本信息进行分类筛选,采用SPSS 27.0软件对数据进行统计分析。以DRG分组为KC19的患者基本信息为自变量,以患者住院费用为因变量,采用Kruskal-Wallis秩和检验方法进行单因素分析,以筛选住院费用相关影响因素,采用多元线性回归分析各因素与住院费用的回归系数。
2. 结果
2.1 患者基本资料
共3809例患者纳入本研究。根据KC19组垂体手术患者的病案首页信息进行分析,患者的平均住院费用为36 166.82元,平均住院天数为9.42 d,基本资料详见表 1。其他诊断数量是指被纳入DRG分组的诊断数量,即具有相关编码的诊断数量。如患者A的病案首页信息为:(Z98.8501)垂体术后| (E24.901)皮质醇增多症[库欣综合征]| (I10xx04) 高血压2级| (E07.901)甲状腺肿物| (N20.005)肾结石,则其他诊断数量为5个。手术操作数量是指被纳入DRG分组的手术操作数量,即具有相关编码的手术操作数量,如患者B的病案首页信息为:(07.62002)经蝶骨垂体病损切除术| (07.79001)空蝶鞍填塞术| (03.31002)腰椎穿刺,则手术操作数量为3个。
表 1 KC19组垂体手术患者基本资料(n=3809)类别 例数[n(%)] 性别 男 1519(39.9) 女 2290(60.1) 年龄(岁) <65 3538(92.9) ≥65 271(7.1) 住院天数(d) <5 725(19) 5~10 2169(57) ≥10 915(24) 其他诊断数量(个) <3 1713(45) ≥3 2096(55) 手术操作数量(个) <3 2451(64.3) ≥3 1358(35.7) 应用神经内镜 否 2469(64.8) 是 1340(35.2) 存在MCC/CC 否 2286(60) 是 1523(40) 注:MCC/CC:严重并发症或合并症/并发症或合并症 2.2 患者住院费用影响因素
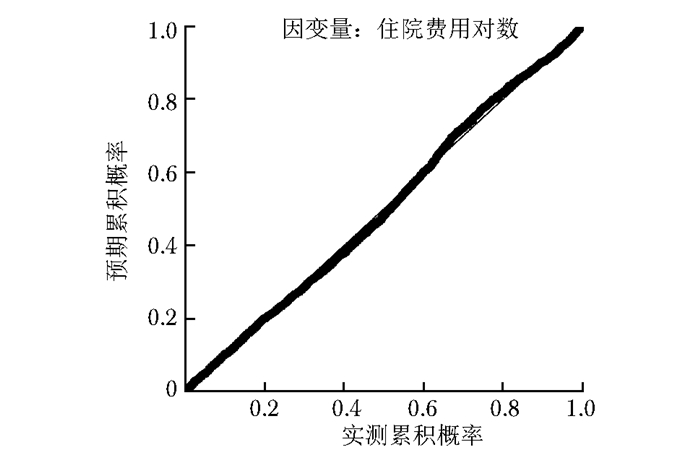
通过单因素分析发现,KC19组垂体手术患者住院费用的影响因素包括性别、住院时长、其他诊断数量、手术操作数量,是否应用神经内镜以及是否存在MCC/CC。以上述影响因素为自变量,以住院费用为因变量进行多元线性回归分析,以三个标准差为界限去掉残差离群值后,得到结果决定系数R2=0.564,各影响因素相应的回归系数详见表 2,所有系数的方差膨胀系数(variance inflation factor,VIF)值均小于5,Durbin-Watson指数为1.627,回归标准化残差的正态P-P图详见图 1,图像大致呈对角直线,表明住院费用对数大致呈正态分布。住院费用的主要影响因素为住院时长,其他影响因素依次为其他诊断数量、手术操作数量、是否应用神经内镜、是否存在MCC/CC和性别。
表 2 KC19组垂体手术患者住院费用主要影响因素指标 非标准化回归系数 标准化回归系数 t值 P值 VIF值 常量项 4.405 676.091 - 性别 0.009 -0.022 -2.051 0.040 1.018 住院天数 0.005 0.565 36.414 <0.001 2.064 其他诊断数量 0.007 0.165 11.959 <0.001 1.625 手术操作数量 -0.011 0.105 7.538 <0.001 1.650 是否存在MCC/CC 0.019 -0.045 -3.593 <0.001 1.321 是否应用神经内镜 -0.005 0.083 7.326 <0.001 1.091 注:MCC/CC:同表 1;VIF:方差膨胀系数 3. 讨论
卫生经济学研究及临床实践均提示住院时长是影响住院费用的重要因素之一[5],DRG分组标准即根据二者的变异系数区分不同的组别。本研究表明,除住院时长外,性别、手术操作数量、其他诊断数量、是否应用神经内镜及是否存在MCC/CC均对KC19组垂体手术患者的住院费用产生影响。除上述因素外,有研究表明患者入院方式(急诊/门诊)和入院状态(一般/紧急/复杂/危重)亦与住院费用存在相关性,是未来进一步研究的方向[5]。DRG组内未综合考虑患者的基础疾病及合并症情况,可能是导致其治疗费用存在巨大差异的原因之一[6]。神经外科收治的患者多为危重症患者,可能是相关疾病分组亏损的重要原因,在此种情况下造成重症患者求医困难,如何进一步探索医改/医保政策从而化解病例组合指数(case mix indicate,CMI)评分低患者的求医难问题是当前亟待解决的难题[7]。因此,更为细化的DRG分组方案乃至个体化医疗将成为未来医疗改革的趋势。
本研究显示,在垂体手术的常见术式中,应用与未应用神经内镜患者的住院费用存在显著统计学差异。在更为复杂的德国DRG分组中,是否应用某种器械操作(如消化内镜是消化道疾病DRG分组的因素)成为多个DRG分组的因素之一[8]。在美国医疗保险严重性诊断相关分组(medicare severity diagnosis related groups,MS-DRG)中,根据是否应用神经内镜将垂体手术细分为两个不同的操作组,研究证实垂体手术患者应用与不应用神经内镜其住院费用存在显著差异[9-12]。
显微内镜手术于20世纪60年代由Jules Hardy引入,其首次采用显微内镜对分泌促肾上腺皮质激素的微腺瘤进行了选择性切除,随着手术的成功以及后续越来越多的研究和报道,显微内镜下切除垂体肿瘤的方法得以建立[13],成为目前应用最广泛的垂体手术术式,而神经内镜垂体手术则是近年来快速发展的新技术。Jankowski等[14]于1992年报道了第1例单纯行神经内镜垂体手术的患者,相较于显微内镜手术,神经内镜手术改善了视觉效果,提高了全肿瘤切除的可能性,降低了肿瘤复发的可能。此外,研究表明,相较于显微内镜手术,神经内镜手术的并发症更少、住院时间更短[15]。
作为新技术,尽管神经内镜手术的单次住院费用高于显微内镜手术,但其远期经济效益高于显微内镜手术[12],且神经内镜手术具有显微内镜手术不能替代的优势和获益,在微创神经内镜手术逐渐成为未来外科治疗趋势的情况下,需综合考虑不同手术方式所用耗材、手术及麻醉时间差异等卫生经济学相关指标。此外,本研究还显示MCC/CC是垂体手术患者住院费用的影响因素之一,而MS-DRG根据此因素将垂体手术和肾上腺手术分为两个不同的DRG组,二者的给付标准亦不同。建议今后国内医疗机构在开展DRG分组的过程中,应纳入上述影响因素将KC19组进行细化。
由于本研究为单中心研究,且仅提取患者的病案首页信息,难以概括患者病情在整个病程发展过程中的具体变化,导致研究结论可能存在一定的局限性。未来应扩大研究范围,纳入来自不同地区、不同医疗机构的病案数据,探寻不同疾病治疗费用的各种影响因素,使疾病分类及医保管理更为精确细致、适合中国国情,以推动国家医疗保障DRG分组快速发展,加快中国医疗管理系统总体水平的快速提升。
4. 小结
本研究通过对北京协和医院神经外科3809例垂体手术患者的病历信息和住院费用进行分析,发现住院时长、其他诊断数量、手术操作数量,是否应用神经内镜、是否存在MCC/CC及性别等因素与住院费用相关。主要影响因素为住院时长,其他影响因素依次为其他诊断数量、手术操作数量、是否应用神经内镜、是否存在MCC/CC和性别。其中,是否应用神经内镜及是否存在MCC/CC是本文讨论的重点,根据本研究和其他国家、地区的经验,建议未来KC19分组应纳入上述影响因素。
2021年6月4日,国务院印发《关于推动公立医院高质量发展的意见》,提出力争通过5年努力,公立医院发展方式从规模扩张转向提质增效,运行模式从粗放型管理转向精细化管理,而精细化管理的基础除自上而下的改革外,自下而上从临床数据出发的研究亦不容忽视。总之,中国的DRG改革正在稳步前进,而更合理的支付方式是符合国情、适合不同地区疾病的分组方法。
作者贡献:杨朗、魏俊吉、张国杰、李春厚负责论文构思;杨朗负责论文撰写;魏俊吉、银锐、文俊贤、常健博、陈亦豪、张笑、马文斌、王任直负责论文审阅及修订。利益冲突:所有作者均声明不存在利益冲突 -
表 1 KC19组垂体手术患者基本资料(n=3809)
类别 例数[n(%)] 性别 男 1519(39.9) 女 2290(60.1) 年龄(岁) <65 3538(92.9) ≥65 271(7.1) 住院天数(d) <5 725(19) 5~10 2169(57) ≥10 915(24) 其他诊断数量(个) <3 1713(45) ≥3 2096(55) 手术操作数量(个) <3 2451(64.3) ≥3 1358(35.7) 应用神经内镜 否 2469(64.8) 是 1340(35.2) 存在MCC/CC 否 2286(60) 是 1523(40) 注:MCC/CC:严重并发症或合并症/并发症或合并症 表 2 KC19组垂体手术患者住院费用主要影响因素
指标 非标准化回归系数 标准化回归系数 t值 P值 VIF值 常量项 4.405 676.091 - 性别 0.009 -0.022 -2.051 0.040 1.018 住院天数 0.005 0.565 36.414 <0.001 2.064 其他诊断数量 0.007 0.165 11.959 <0.001 1.625 手术操作数量 -0.011 0.105 7.538 <0.001 1.650 是否存在MCC/CC 0.019 -0.045 -3.593 <0.001 1.321 是否应用神经内镜 -0.005 0.083 7.326 <0.001 1.091 注:MCC/CC:同表 1;VIF:方差膨胀系数 -
[1] 国家医疗保障局. 关于印发疾病诊断相关分组(DRG)付费国家试点技术规范和分组方案的通知[EB/OL ]. (2019-10-24)[2022-08-26]. http://www.nhsa.gov.cn/art/2019/10/24/art_52_1875.html. [2] Daly AF, Beckers A. The Epidemiology of Pituitary Adenomas[J]. Endocrinol Metab Clin North Am, 2020, 49: 347-355. DOI: 10.1016/j.ecl.2020.04.002
[3] 国家医疗保障局. 医疗保障疾病诊断相关分组(CHS-DRG)细分组方案(1.0版)[EB/OL ]. (2020-06-18)[2022-08-26]. http://www.nhsa.gov.cn/art/2020/6/18/art_37_3240.html. [4] Lee CC, Kimmell KT, Lalonde A, et al. Geographic variation in cost of care for pituitary tumor surgery[J]. Pituitary, 2016, 19: 515-521. DOI: 10.1007/s11102-016-0738-x
[5] 李秀梅, 刘理, 胡海源, 等. DRG支付下脑卒中患者住院费用控制研究[J]. 卫生经济研究, 2022, 1: 44-47. https://www.cnki.com.cn/Article/CJFDTOTAL-WSJJ202201013.htm [6] Vaughan-Sarrazin M, Bayman L, Rosenthal G, et al. The business case for the reduction of surgical complications in VA hospitals[J]. Surgery, 2011, 149: 474-483. DOI: 10.1016/j.surg.2010.12.004
[7] 廖慧群, 麦紫娟, 廖彩霞. 收治病种结构对医院CMI值的影响[J]. 中国病案, 2022, 23: 10-12. https://www.cnki.com.cn/Article/CJFDTOTAL-ZGBN202201005.htm [8] Institut für das Entgeltsystem im Krankenhaus. aG-DRG German Diagnosis Related Groups Version 2022 Definitionshandbuch Kompaktversion[EB/OL]. (2022-01-26)[2022-08-26]. https://www.g-drg.de/aG-DRG-System_2022/Definitionshandbuch/Definitionshandbuch_20222.
[9] Centers for Medicare & Medicaid Services. ICD/-10-CM/PCS MS-DRG v39.1 Definitions Manual[EB/OL]. (2021-11-16)[2022-08-26]. https://www.cms.gov/icd10m/version39-fullcode-cms/fullcode_cms/P0001.html.
[10] Eseonu CI, ReFaey K, Garcia O, et al. Comparative Cost Analysis of Endoscopic versus Microscopic Endonasal Transsphenoidal Surgery for Pituitary Adenomas[J]. J Neurol Surg B Skull Base, 2018, 79: 131-138. DOI: 10.1055/s-0037-1604484
[11] Ament JD, Yang Z, Khatchadourian V, et al. Cost-Effectiveness of Endoscopic Versus Microscopic Transsphenoidal Surgery for Pituitary Adenoma[J]. World Neurosurg, 2018, 110: e496-e503. DOI: 10.1016/j.wneu.2017.11.046
[12] Jethwa PR, Patel TD, Hajart AF, et al. Cost-Effectiveness Analysis of Microscopic and Endoscopic Transsphenoidal Surgery Versus Medical Therapy in the Management of Microprolactinoma in the United States[J]. World Neurosurg, 2016, 87: 65-76. DOI: 10.1016/j.wneu.2015.10.090
[13] Hardy J. Transphenoidal microsurgery of the normal and pathological pituitary[J]. Clin Neurosurg, 1969, 16: 185-217. DOI: 10.1093/neurosurgery/16.CN_suppl_1.185
[14] Jankowski R, Auque J, Simon C, et al. Endoscopic pituitary tumor surgery[J]. Laryngoscope, 1992, 102: 198-202.
[15] Tabaee A, Anand VK, Barrón Y, et al. Endoscopic pituitary surgery: a systematic review and meta-analysis[J]. J Neurosurg, 2009, 111: 545-554. DOI: 10.3171/2007.12.17635
-
期刊类型引用(7)
1. 王栎垚,毛国育. 公立A医院运用DRG对临床科室的运营管理研究. 医学信息. 2023(04): 52-56 .  百度学术
百度学术
2. 李梦滢,顼晋昆,杨菁. 基于归纳法和专家咨询法的CHS—DRG合并症、并发症分组探索——以UPPP手术在DB33和DB35入组为例. 中国医疗保险. 2023(09): 86-93 .  百度学术
百度学术
3. 曾凡伟,任国娇. DRG视角下北京市3次医改对冠心病介入患者住院费用的影响. 现代医药卫生. 2023(19): 3406-3410 .  百度学术
百度学术
4. 宋康,刘新靓,罗小霞,张志彬,潘卫兵,李准,黎浩. 基于决策树模型的梗阻性肾盂积水患者住院费用及病例组合优化研究. 华西医学. 2023(10): 1530-1536 .  百度学术
百度学术
5. 丁敬美,韩磊,杜进兵. 武汉市DRG入组病例的费用倍率特征分析. 卫生经济研究. 2023(12): 28-32 .  百度学术
百度学术
6. 伍渊麟,刘耀,甘岚澜,向贵圆,李晨,陈世耕,鲜秋婉. DRG支付方式下EB19组胸部大手术患者住院费用的影响因素研究. 重庆医学. 2023(23): 3665-3668 .  百度学术
百度学术
7. 聂晓静,付豪斐,白荷荷,李亚萍,王金萍. 糖尿病患者DRG分组效果及住院费用影响因素分析. 中国药房. 2023(24): 3020-3024 .  百度学术
百度学术
其他类型引用(1)

 作者投稿
作者投稿 专家审稿
专家审稿 编辑办公
编辑办公 邮件订阅
邮件订阅 RSS
RSS

 下载:
下载: