Expert Consensus on the Preoperative Geriatric Assessments of Elderly Patients with Glioma (2019)
-
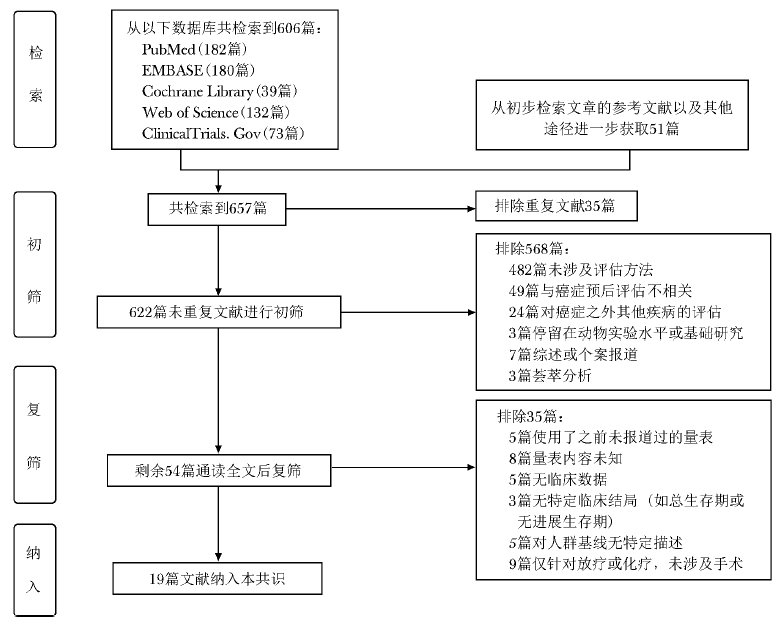
摘要: 胶质瘤是成年人中最常见的原发性脑肿瘤,其中以胶质母细胞瘤(glioblastoma,GBM)恶性程度最高。目前针对胶质瘤患者的治疗方式主要包括手术切除、放疗和化疗,而GBM的治疗策略,特别是老年GBM患者的治疗策略,尤其是手术方式,常因其自身特点而产生差异。术前系统而全面的评估有助于总结老年GBM的临床特点及相应诊疗方案,为临床医生提供更全面的患者信息,以更加准确判断老年患者对手术的耐受程度以及预测患者预后。本专家共识在对最新研究证据进行系统回顾的基础上,将目前已广泛应用的胶质瘤术前评估项目及评估工具进行总结,初步建立中国老年胶质瘤患者术前评估体系。Abstract: Glioma is the most common primary brain tumor in adults, among which glioblastoma (GBM) is the most malignant. At present, the therapeutic regimen for patients with glioma mainly includes surgery, radiotherapy, and chemotherapy. However, the treatment strategy for elderly patients with GBM often varies because of their characteristics. A systematic and comprehensive assessment before the operation will be helpful to summarize clinical characteristics of elderly patients with GBM, and can provide clinicians with more comprehensive clinical information in order to evaluate the patient's tolerance to surgery and predict the prognosis. Based on a systematic review of the latest research, this expert consensus summarizes the most widely used and studied tools of preoperative assessment of glioma, and initially establishes a preoperative evaluation system for elderly patients with glioma in China.
-
Keywords:
- glioma /
- preoperative assessment /
- geriatric
-
近年来,关节炎性疾病的发病率在全球范围内显著增长。其中,以慢性非创伤性关节炎性疾病增长较为明显,包括骨关节炎(osteoarthritis,OA)和类风湿关节炎(rheumatoid arthritis,RA)两大类。关节慢性炎性病变是最常见的非外伤性活动受限和致残原因[1-2]。研究表明,早期药物治疗可有效防止关节炎性病变恶化,并在一定程度上减少其后期功能受限和残疾的发生[3]。然而,早期关节炎性病变的临床症状并不显著,常规影像学检查的诊断灵敏度欠佳,难以对关节炎进行治疗指导及预后预测。新型成像技术可对小关节进行高分辨率成像,实现对关节炎性疾病的诊断及预后评估,有助于临床诊疗前移,精准指导治疗,改善患者的整体预后。本文重点介绍光声成像(photoacoustic imaging, PAI)技术在关节炎性疾病中应用的可行性及其潜在临床价值。
1. 关节炎性疾病常用的影像学评价方法
目前慢性关节炎常用的影像学诊断评估方法包括X线、CT、MRI及超声,上述成像技术多用于评估OA及RA受损关节。关节炎的影像学特征基于其病理学改变而产生,如OA病变关节的关节间隙狭窄、软骨下硬化和软组织骨化,RA病变关节内的滑膜炎性病变(增厚及充血)、肌腱及周围组织炎性病变、滑囊炎性病变及骨质侵蚀等。X线对于诊断骨损伤有较高的准确度,1987年美国风湿病学会制定的RA指南认为X线是诊断RA的影像学金标准,并对其作出评级[4]。但因X线分辨率不高而限制了其在关节炎性疾病早期诊断中的应用。CT作为一种辅助检查手段,通过多层面显像,可显示受损关节的软骨下损害、软组织钙化及骨侵蚀。MRI对软组织具有较高的分辨率,是关节炎性疾病广泛应用的影像诊断方法,通过多序列多层面关节组织成像,可显示关节炎的早期改变,且注射增强造影剂后可进一步增加其灵敏度[5]。高频超声可显示炎性关节周围组织的改变,包括滑膜炎、腱鞘炎、腱周炎、滑囊炎等,还可评估关节炎性疾病中常出现的关节腔积液及骨质侵蚀特征,灰阶超声的半定量评分评估炎性活动度也在部分研究中得到了应用。随着多普勒技术的广泛应用,超声在关节炎性疾病中的诊断价值提高,通过显示关节炎性区域的血流情况,采用半定量评估方式对疾病活动度进行评估[6]。
近年来,随着影像学技术的发展,新型光学成像技术陆续应用于临床,包括弥散性光成像(diffuse optical imaging, DOI)、荧光及生物荧光成像,为关节炎性疾病的早期诊断带来了新的曙光[7-8]。多波长DOI可计算氧合血红蛋白和非氧合血红蛋含量,以提示病变关节的功能改变,如充血、新生血管形成及缺氧等。超声造影(contrast-enhanced ultrasound,CEUS) 是近年来临床推广的超声新技术之一,研究证明CEUS可对滑膜炎性病变进行探查,并定量/半定量评价疾病活动度及开展关节炎分子成像[9]。
常规及新型影像学技术可进行关节形态学、微血管及功能成像,对关节病变诊断有较好的准确度和灵敏度,但尚无可同时实现无创性形态学、微血管及功能成像,又兼具较高小关节成像分辨率的影像学方法。而PAI可实现同一影像平台上无创高分辨率小关节成像及结构与功能的定量分析,具有潜在的临床应用价值。
2. 光声成像技术原理与成像系统
PAI是一种新型无创性光学成像技术,其原理为光声效应,即在可调节范围内将光信号转换为声信号进行成像。光声效应最早于1886年由Alexander Graham Bell提出,当组织被短脉冲波长的激光照射后内部温度上升,产生热弹性膨胀,在此过程中产生一段宽频带的超声波;该段超声波可被配置有压电元件的超声探头接收,通过图像重建及处理后,声信号被转换为光声图像[10]。PAI结合了光显像和超声成像的优点,在反映组织光学特性的同时,达到较高的显像深度和空间分辨率。典型的光声系统主要由激光发射仪器、光传输线路及超声信号接收处理器组成,主要仪器类型包括光声计算机断层成像(photoacoustic computed tomography, PACT)、光声显微成像(photoacoustic microscopy, PAM)及光声内镜成像(photoacoustic endoscopy, PAE)[11]。其中,PACT是较为成熟的PAI技术,通过改变探头排列方式或旋转模式及复杂的图像处理后可将光声信号转化为2D及3D图像[12]。
通过内源性光显像剂,如氧合血红蛋白、脱氧血红蛋白、黑色素、水和脂质等,PAI可同时实现解剖学成像和功能成像。利用多波长PAI显示氧合血红蛋白及脱氧血红蛋白,可计算血氧饱和度等反映组织功能的参数[13]。搭载特异性分子的外源性光显像剂,如吲哚菁绿、纳米金颗粒、单壁纳米碳管等,可实现分子PAI[14]。
3. 光声成像技术在关节成像中的发展
PAI具有较高的空间分辨率和显像深度,适用于关节成像,特别是小关节。PAI不仅显示关节解剖学结构,还可对其功能参数进行定量测定,具有较好的临床转化前景。近10年来,随着PAI技术的发展,其在关节成像中的研究逐渐增多。
3.1 光声计算机断层成像
近年来,国外研究团队开发了针对关节成像的PACT系统及相应动物模型,并开展了临床前实/试验(表 1)。2006年,密歇根大学研究团队最先开发了专门用于关节成像的3D PACT系统,并在鼠尾关节动物模型及人体(尸体)上进行了试验[15]。该系统利用宽频超声探头绕关节进行弓形旋转,经处理后生成3D图像,可清晰显示关节周围组织(如皮肤、脂肪、肌肉、血管、滑膜等),并可反映组织内血红蛋白分布情况[16]。研究者应用该系统定量测定关节炎模型大鼠踝关节内的光声信号,发现其局部光声信号增强[17]。佛罗里达大学研究团队同期也研发了定量3D PACT PAI系统,并进行了关节模型和人体在体试验[18-20],发现光声三维关节成像与MRI图像具有一致性。该团队在后期研究中采用半环形超声探头列阵对系统进行改进,使其更适用于人体关节成像[21]。van Es等[22]设计了配有半环形超声探头列阵的PACT系统,对人体手指关节、血管进行显像,发现其可清晰显示指间关节周围的甲床、皮肤及皮下软组织层血管,且与组织学相符合。Ermilov等[23]开发了针对关节微血管成像的PACT系统,通过360°旋转实现三维显像,对关节微血管具有较高的分辨率,同时可通过快速PAI显示小血管的温度调节反应。
上述研究表明,PACT可较好地显示关节周围组织的形态结构,可显示普通超声难以显示的关节内软骨和骨,对微血管和新生血管的显示率较高,这一特点对关节疾病具有重要诊断价值。
3.2 双模态光声/超声成像系统
光声信号和超声信号均由超声传感器(探头)接收,经图像后处理后可同时得到两种成像方式的显像结果,并使光声图像叠加在灰阶超声图像上,实现双模态光声/超声(photoacoustic/ultrasound, PA/US)成像,是现阶段常见的成像系统之一。双模态PA/US成像系统通过多波段PACT和超声成像,获取目标组织解剖功能信息,此种多模态成像方法也是现阶段关节PAI研究的热点,相关研究见表 2。
表 2 双模态PA/US成像系统相关研究仪器 研究结果 年份 PACT/USCT[24] 多波长显示人体手指关节内结构 2016 PACT/USCT[25] 人体手指关节结构及微血管显像 2017 PA系统+具备L10-5探头商用超声仪器[26-28] 关节炎小鼠踝关节治疗前后光声信号变化; 人体手指关节结构及微血管显像 2011 2012 2013 具备手持光声探头PA/US成像[30-31] 健康人、关节炎患者手指关节结构及微血管显像 2014 2017 具备手持光声探头PA/US成像[33] 关节炎患者手指微血管显像、双波长血氧饱和度测定 2017 PACT/USCT:光声计算机断层成像/超声计算机断层成像;PA:光声;PA/US:光声/超声成像 有研究将PACT和超声计算机断层成像(ultrasound tomography,USCT)整合至同一影像平台,形成PACT/USCT双模态成像系统,结合光声信号和灰阶超声图像,对人体手指局部结构具有更清晰的认识,可达到诊断疾病的目的[24-25]。目前,较常见的光声与超声成像结合方法则是构建一体化的双模态PA/US成像系统。
由于超声影像检查的高性价比和便携性,其在世界范围内得以广泛应用,而独立PAI系统因体积较大、设计复杂、价格昂贵,其临床应用受到一定限制。为使光声技术进一步向临床转化,研究人员将光声技术整合于商品化超声影像系统,构建了新型一体化双模态PA/US成像系统。这种双模态成像系统将光声信号整合至超声灰阶图像,利用超声灰阶图像指导光声信号的定性分析和定量评估,在实现PAI的基础上同时兼具商品化超声影像系统稳定性的优点。Wang等[26]首先将PAI技术整合于商用超声仪器,并应用此双模态成像系统对关节炎模型小鼠的踝关节进行1064 nm和532 nm双波长检查,可在炎性病变区域内探测到显著升高的光声信号[27],接受靶向药物治疗后,关节炎小鼠的光声信号出现明显下降[28]。该团队在此基础上进一步对双模态PA/US成像系统进行了适于人体关节成像的改造,并获得了清晰的人体手指关节光声图像[29]。
将光传输系统进一步整合至超声探头,形成一体化便携式PA/US探头,更符合临床医生的使用习惯,便于临床转化及推广应用,目前已成为多功能PA/US成像系统的研究重点。Daoudi[30]等将光传输设施整合至超声探头内,开发出一种简便的光声系统超声探头,可同时获取清晰的超声及光声图像。为进一步证实其临床潜在应用价值,研究者开展了相关临床前研究,发现关节炎区域光声信号显著增强[31]。密歇根大学研究团队在此基础上开发了具有手持光声探头的双模态PA/US成像系统,并应用该系统对关节炎患者和健康对照组的手指关节进行580 nm单波长显像和532 nm、1064 nm双波长显像,发现关节炎患者的血流及血氧饱和度与健康对照组存在显著差异[32],证实其可对充血、缺氧等炎性关节功能改变进行定量诊断[33]。该团队进一步使用LED作为双模态PA/US成像系统光源,成功获取高信噪比的PA/US实时整合图像,可显示最大直径为5 mm的手指微血管,并获取手指关节的血氧定量结果,该研究成果对PAI在关节炎中的临床应用推广具有较大价值[34]。
自2015年起,北京协和医院超声医学科研究团队和北京大学、深圳迈瑞生物医疗电子股份有限公司合作,致力于开发配置手持光声探头的PA/US多功能影像一体化平台,将光声系统部分整合至临床应用的高端超声成像探头(L9-3U, 深圳迈瑞生物医疗电子股份有限公司),应用该仪器可同时检测光声和超声信号,并获得光声与超声的叠加图像,该影像平台已成功开展了甲状腺结节和乳腺结节诊断的临床前期研究[35]。目前,该团队进一步开展了RA的临床研究,发现多模态PA/US对小关节内滑膜组织微血管有较好地显示,且与临床评分具有较好的相关性,可对RA患者的小关节进行全面评价,有望在疾病活动度、随访及预后预测等方面发挥临床应用价值。
3.3 结合超声及其他医学影像技术的多重成像系统
PAI技术还可与光散射断层成像技术(diffused optical tomography, DOT)整合至同一影像平台。Xi等[36]将PACT和DOT整合于一体化成像平台,利用探头列阵接收光声信号,并通过有限元图像重建程序处理弥散光信号,从而同时获取PACT和DOT成像,并进行图像叠加融合。研究表明,人体关节周围组织和骨骼可被PACT和DOT显示,该系统可应用于关节炎症的评估[36]。
4. 外源性光声造影剂在关节成像中的应用
在开发关节PAI仪器的基础上,研究者采用外源性光声造影剂,将关节PAI技术的应用扩展到了分子成像水平。一项研究将抗肿瘤坏死因子结合在外源性光声造影剂纳米金颗粒上,注射至关节炎模型小鼠的尾关节,在600 nm波长下进行PAI,发现其关节内信号强度明显高于未注射造影剂的对照组[37]。
半萘酚罗丹荧(Seminaphthorhodafluor, SNARF-5F)是一种特殊的pH灵敏度染料,可与纳米探针结合检测局部组织pH值,该分子探针亦可用于关节PAI[38]。将分子探针复合物注射至关节局部组织后,可计算光声信号、检测组织局部pH值,对关节炎性疾病有一定的辅助诊断价值。
在外源性光声造影剂近红外区荧光团标记树枝状聚甘油聚阴离子硫酸, 形成L-选择素/P-选择素(L-selectin/P-selectin)特异性复合物,可靶向监测炎性反应。将该炎症特异性探针局部注射至关节炎模型小鼠的膝关节及踝关节进行PAI,发现其光声信号强度明显高于健康小鼠,且与增强MRI及组织学结果相一致[39]。
另有研究发现,用于治疗OA的抗炎药氯法齐明(Clofazimine,CFZ)在450 nm时光吸收系数较高,亦可用于PAI。CFZ在巨噬细胞内聚集,可用于指导细胞特异性诊断和治疗的监测。光声显微成像技术证实CFZ可应用于光声分子成像,并进一步在双模态PA/US成像系统上对注射CFZ的模型、动物模型及尸体手指关节进行显像,均可得到满意的光声信号,提示PAI技术可用于CFZ治疗OA的药物监测[40]。
5. 小结与展望
PAI技术是一种新型、无创性医学影像学检测手段,其在关节成像中的应用价值已被相关研究证实,在关节炎性疾病的诊断、疗效监测等方面具有临床应用前景,其中PAI仪器与手持式超声探头的结合是未来临床转化型成像设备的重要研究方向。
作为一种新型影像学技术,PAI的图像分辨率尚低于目前临床常用的高度完善的影像学手段,未来尚需进一步优化改进、提高信噪比和分辨率,并消除伪像[41-42]。目前PAI技术在关节炎性疾病中应用的临床研究较少,且多数研究尚处于起步阶段,纳入病例数较少,对其临床价值论证不足。此外,将PAI技术与其他影像技术进行对比研究尚有欠缺,尚未对其优劣性作出评价。对于PAI技术测定血氧饱和度的功能成像,仍需进一步扩大样本量验证其对关节炎性疾病的诊断价值。
利益冲突 无 -
表 1 老年胶质瘤患者手术治疗方案相关文献
作者 发表时间 平均年龄(岁) 性别(男/女, n) 干预措施 结果 随访时间(年) 研究类型 试验组 对照组 Gupta等[7] 2018年 6.3 23/27 活检术 无 50例弥漫内生性脑干胶质瘤患者中,46例成功获得活检组织并指导进一步诊治 随访至死亡 单臂临床研究 Kellermann等[8] 2017年 74 129/101 立体定向活检术 无 239例老年胶质瘤患者中230例接受了立体定向活检术,其中222例成功取得组织学诊断并有171例接受了后续辅助治疗 1 回顾性研究 Tanaka等[9] 2013年 74.1 61/44 立体定向活检术 常规外科手术 接受立体定向活检术的患者术后出血风险较常规外科手术高 5 回顾性研究 表 2 老年胶质瘤患者术前评估相关文献
作者 发表时间 平均年龄(岁) 性别(男/女, n) 干预措施 结果 平均随访时间(年) 研究类型 评估项目 试验组 对照组 Johnson等[17] 2012年 53.9 55/36 WAIS-R, WAIS-Ⅲ, HVLT-R量表 无 认知功能中的执行力与注意力均与胶质母细胞瘤患者的预后有关 9 回顾性研究 认知功能 Rambeau等[20] 2018年 78 25/41 MMSE量表 MoCA量表 MoCA量表比MMSE量表在评估认知功能方面更加精确 1 临床对照研究 认知功能 Fiorentino等[21] 2012年 72 17/18 - - 对合并症的评估也是对老年胶质母细胞瘤患者预后预测十分有效的工具 6 单臂临床研究 合并症 Ening等[22] 2015年 62 117/116 - - 年龄越大、KPS越低、CCI越高,则难治性胶质母细胞瘤患者的总生存期或肿瘤无进展生存期越短 5 回顾性研究 合并症 Villani等[23] 2019年 73 70/48 - - CIRS合并症指数得分越高,老年胶质母细胞瘤患者手术、放/化疗或单纯放疗的预后越差 1 前瞻性队列研究 合并症 Cloney等[24] 2015年 NA NA - - 虚弱的老年胶质母细胞瘤患者更不倾向于接受手术治疗,其卧床时间较长,且术后并发症发生率较高 12 回顾性研究 虚弱 Peters等[26] 2014年 50 161/76 - - 疲惫独立影响复发高级别胶质瘤患者的预后,疲惫感越强则预后越差;生活质量并非预后的独立预测因素 2 前瞻性队列研究 疲惫与生活质量 Borg等[42] 2011年 60.1 419/266 - - 术前低蛋白血症患者较正常者术后生存期短 10 回顾性研究 实验室检验 He等[49] 2017年 44 197/129 - - 术前高纤维蛋白原和低血胆红素的新诊断高级别患者肿瘤进展和死亡风险更大 2 单臂临床研究 实验室检验 -:未分组评估;WAIS-R:Wechsler成人智力量表(修订版); HVLT-R:霍普金斯词语学习测验(修订版); MMSE:简易精神状态检查; MoCA:蒙特利尔认知评估; KPS:卡式评分; CCI:查尔森合并症指数;CIRS:累积疾病评分量表 表 3 老年胶质瘤患者术前评估筛查方法相关文献
作者 发表时间 平均年龄(岁) 性别(男/女,n) 测量方法/量表 结果 研究类型 评估项目 Kane等[54] 2012年 NA NA 通过8项老年综合征指标(合并症、认知功能障碍、虚弱、残疾、营养不良、内分泌紊乱、慢性炎症等)评估 对老年综合征的评估对年龄稍小老龄患者意义更大;对年龄较大老龄患者意义不大 系统综述 老年综合征 Soubeyran等[11] 2014年 78 434/1001 用G8量表和老年人受伤情况调查(第13版)量表对老年癌症患者进行多维度老年评估,包括特异度、敏感度、阳性预测值、阴性预测值,1年生存期预测等 G8量表的敏感度较VES-13高,但特异度则比VES-13低。G8量表评分可以独立预测老年癌症患者的1年生存期 前瞻性队列研究 多维度老年学评估 Svendsboe等[56] 2015年 74.9 72/114 RSS,认知功能(MMSE、CDR-SOB),精神心理状态(NPI、MADRS、UPDRS),其他变量因素(CIRS、RDRS-2) 照护者在阿尔茨海默病和路易氏痴呆患者的发病初期,可能会有轻到中度的照护者负担问题,同样也会有精神问题的可能 横断面研究 照护提供者 RSS:照护者负担量表;MMSE:简易精神状态量表;CDR-SOB:临床痴呆评定量表;NPI:神经精神症状问卷;MADRS:蒙哥马利和阿斯伯格抑郁症等级量表;UPDRS:帕金森分级量表;CIRS:累积疾病评分量表;RDRS-2:快速残疾评定量表 -
[1] Ostrom QT, Gittleman H, Xu J, et al. CBTRUS Statistical Report: Primary Brain and Other Central Nervous System Tumors Diagnosed in the United States in 2009-2013[J]. Neuro Oncol, 2016, 18:v1-v75. DOI: 10.1093/neuonc/now207
[2] 国家卫生健康委员会医政医管局.脑胶质瘤诊疗规范(2018年版)[J].中华神经外科杂志, 2019, 35:217-239. DOI: 10.3760/cma.j.issn.1001-2346.2019.03.001 [3] Almenawer SA, Badhiwala JH, Alhazzani W, et al. Biopsy versus partial versus gross total resection in older patients with high-grade glioma: a systematic review and meta-analysis[J]. Neuro Oncol, 2015, 17:868-881. DOI: 10.1093/neuonc/nou349
[4] Extermann M, Hurria A. Comprehensive geriatric assessment for older patients with cancer[J]. J Clin Oncol, 2007, 25:1824-1831. DOI: 10.1200/JCO.2007.10.6559
[5] Martinez R, Janka M, Soldner F, et al. Gross-total resection of malignant gliomas in elderly patients: implications in survival[J]. Zentralbl Neurochir, 2007, 68:176-181. DOI: 10.1055/s-2007-985851
[6] Vuorinen V, Hinkka S, Farkkila M, et al. Debulking or biopsy of malignant glioma in elderly people-a randomised study[J]. Acta Neurochir (Wien), 2003, 145:5-10. DOI: 10.1007/s00701-002-1030-6
[7] Gupta N, Goumnerova LC, Manley P, et al. Prospective feasibility and safety assessment of surgical biopsy for patients with newly diagnosed diffuse intrinsic pontine glioma[J]. Neuro Oncol, 2018, 20:1547-1555. DOI: 10.1093/neuonc/noy070
[8] Kellermann SG, Hamisch CA, Ruess D, et al. Stereotactic biopsy in elderly patients: risk assessment and impact on treatment decision[J]. J Neurooncol, 2017, 134:303-307. DOI: 10.1007/s11060-017-2522-9
[9] Tanaka S, Meyer FB, Buckner JC, et al. Presentation, management, and outcome of newly diagnosed glioblastoma in elderly patients[J]. J Neurosurg, 2013, 118:786-798. DOI: 10.3171/2012.10.JNS112268
[10] Mohile SG, Dale W, Somerfield MR, et al. Practical Assessment and Management of Vulnerabilities in Older Patients Receiving Chemotherapy: ASCO Guideline for Geriatric Oncology[J]. J Clin Oncol, 2018, 36:2326-2347. DOI: 10.1200/JCO.2018.78.8687
[11] Soubeyran P, Bellera C, Goyard J, et al. Screening for vulnerability in older cancer patients: the ONCODAGE Prospective Multicenter Cohort Study[J]. PLoS One, 2014, 9:e115060. DOI: 10.1371/journal.pone.0115060
[12] Overcash JA, Beckstead J, Extermann M, et al. The abbreviated comprehensive geriatric assessment (aCGA): a retrospective analysis[J]. Crit Rev Oncol Hematol, 2005, 54:129-136. DOI: 10.1016/j.critrevonc.2004.12.002
[13] Saliba D, Elliott M, Rubenstein LZ, et al. The Vulnerable Elders Survey: a tool for identifying vulnerable older people in the community[J]. J Am Geriatr Soc, 2001, 49:1691-1699. DOI: 10.1046/j.1532-5415.2001.49281.x
[14] Kim JW, Kim SH, Lee YG, et al. Prospective Validation of The Korean Cancer Study Group Geriatric Score (KG)-7, a Novel Geriatric Screening Tool, in Older Patients with Advanced Cancer Undergoing First-line Palliative Chemotherapy[J]. Cancer Res Treat, 2019. doi: 10.4143/crt.2018.451. [Epub ahead of print].
[15] Rowbottom L, Loucks A, Jin R, et al. Performance of the Vulnerable Elders Survey 13 screening tool in identifying cancer treatment modification after geriatric assessment in pre-treatment patients: A retrospective analysis[J]. J Geriatr Oncol, 2019, 10:229-234. DOI: 10.1016/j.jgo.2018.10.018
[16] Perry JR, Laperriere N, O'Callaghan CJ, et al. Short-Course Radiation plus Temozolomide in Elderly Patients with Glioblastoma[J]. N Engl J Med, 2017, 376:1027-1037. DOI: 10.1056/NEJMoa1611977
[17] Johnson DR, Sawyer AM, Meyers CA, et al. Early measures of cognitive function predict survival in patients with newly diagnosed glioblastoma[J]. Neuro Oncol, 2012, 14:808-816. DOI: 10.1093/neuonc/nos082
[18] Hansson L, Lithell H, Skoog I, et al. Study on COgnition and Prognosis in the Elderly (SCOPE): baseline characteristics[J]. Blood Press, 2000, 9:146-151. DOI: 10.1080/080370500453483999
[19] Nasreddine ZS, Phillips NA, Bedirian V, et al. The Montreal Cognitive Assessment, MoCA: a brief screening tool for mild cognitive impairment[J]. J Am Geriatr Soc, 2005, 53:695-699. DOI: 10.1111/j.1532-5415.2005.53221.x
[20] Rambeau A, Beauplet B, Laviec H, et al. Prospective comparison of the Montreal Cognitive Assessment (MoCA) and the Mini Mental State Examination (MMSE) in geriatric oncology[J]. J Geriatr Oncol, 2019, 10:235-240. DOI: 10.1016/j.jgo.2018.08.003
[21] Fiorentino A, Caivano R, Chiumento C, et al. Comorbidity assessment and adjuvant radiochemotherapy in elderly affected by glioblastoma[J]. Med Oncol, 2012, 29:3467-3471. DOI: 10.1007/s12032-012-0246-4
[22] Ening G, Osterheld F, Capper D, et al. Charlson comorbidity index: an additional prognostic parameter for preoperative glioblastoma patient stratification[J]. J Cancer Res Clin Oncol, 2015, 141:1131-1137. DOI: 10.1007/s00432-014-1907-9
[23] Villani V, Tanzilli A, Telera SM, et al. Comorbidities in elderly patients with glioblastoma: a field-practice study[J]. Future Oncol, 2019, 15:841-850. DOI: 10.2217/fon-2018-0524
[24] Cloney M, D'Amico R, Lebovic J, et al. Frailty in Geriatric Glioblastoma Patients: A Predictor of Operative Morbidity and Outcome [J]. World Neurosurg, 2016, 89:362-367. DOI: 10.1016/j.wneu.2015.12.096
[25] Basic D, Shanley C. Frailty in an older inpatient population: using the clinical frailty scale to predict patient outcomes[J]. J Aging Health, 2015, 27:670-685. DOI: 10.1177/0898264314558202
[26] Peters KB, West MJ, Hornsby WE, et al. Impact of health-related quality of life and fatigue on survival of recurrent high-grade glioma patients[J]. J Neurooncol, 2014, 120:499-506. DOI: 10.1007/s11060-014-1574-3
[27] Aaronson NK, Ahmedzai S, Bergman B, et al. The European Organization for Research and Treatment of Cancer QLQ-C30: a quality-of-life instrument for use in international clinical trials in oncology[J]. J Natl Cancer Inst, 1993, 85:365-376. DOI: 10.1093/jnci/85.5.365
[28] Aapro M, Extermann M, Repetto L. Evaluation of the elderly with cancer[J]. Ann Oncol, 2000, 11 Suppl 3:223-229.
[29] Jager-Wittenaar H, Dijkstra PU, Vissink A, et al. Malnutrition in patients treated for oral or oropharyngeal cancer—prevalence and relationship with oral symptoms: an explorative study[J]. Support Care Cancer, 2011, 19:1675-1683. DOI: 10.1007/s00520-010-1001-z
[30] Gielda BT, Mehta P, Khan A, et al. Weight gain in advanced non-small-cell lung cancer patients during treatment with split-course concurrent chemoradiotherapy is associated with superior survival[J]. Int J Radiat Oncol Biol Phys, 2011, 81:985-991. DOI: 10.1016/j.ijrobp.2010.06.059
[31] 李璞, 赵理.南阳市敬老院230例老人营养状况调查[J].中国老年学杂志, 2004, 24:747-748. DOI: 10.3969/j.issn.1005-9202.2004.08.036 [32] 周丽平, 孙建萍, 杨支兰, 等.养老机构老年人营养管理研究进展[J].中国老年学杂志, 2016, 36:753-755. DOI: 10.3969/j.issn.1005-9202.2016.03.106 [33] Rubenstein LZ, Harker JO, Salva A, et al. Screening for undernutrition in geriatric practice: developing the short-form mini-nutritional assessment (MNA-SF) [J]. J Gerontol A Biol Sci Med Sci, 2001, 56:M366-M372. DOI: 10.1093/gerona/56.6.M366
[34] Guigoz Y, Lauque S, Vellas BJ. Identifying the elderly at risk for malnutrition. The Mini Nutritional Assessment[J]. Clin Geriatr Med, 2002, 18:737-757. DOI: 10.1016/S0749-0690(02)00059-9
[35] Kristensen SD, Knuuti J, Saraste A, et al. 2014 ESC/ESA Guidelines on non-cardiac surgery: cardiovascular assess-ment and management: The Joint Task Force on non-cardiac surgery: cardiovascular assessment and management of the European Society of Cardiology (ESC) and the European Society of Anaesthesiology (ESA) [J]. Eur Heart J, 2014, 35:2383-2431. DOI: 10.1093/eurheartj/ehu282
[36] Fleisher LA, Fleischmann KE, Auerbach AD, et al. 2014 ACC/AHA guideline on perioperative cardiovascular evaluation and management of patients undergoing noncardiac surgery: a report of the American College of Cardiology/American Heart Association Task Force on practice guidelines[J]. J Am Coll Cardiol, 2014, 64:e77-e137. DOI: 10.1016/j.jacc.2014.07.944
[37] 朱鸣雷, 黄宇光, 刘晓红, 等.老年患者围手术期管理北京协和医院专家共识[J].协和医学杂志, 2018, 9:36-41. DOI: 10.3969/j.issn.1674-9081.2018.01.008 [38] Kaya T, Sipahi S, Karacaer C, et al. Evaluation of nutritional status with different methods in geriatric hemodialysis patients: impact of gender[J]. Int Urol Nephrol, 2014, 46:2385-2391. DOI: 10.1007/s11255-014-0776-0
[39] Lin MY, Liu WY, Tolan AM, et al. Preoperative serum albumin but not prealbumin is an excellent predictor of postoperative complications and mortality in patients with gastrointestinal cancer[J]. Am Surg, 2011, 77:1286-1289. https://www.ncbi.nlm.nih.gov/pubmed/22127071
[40] Fujii T, Sutoh T, Morita H, et al. Serum albumin is superior to prealbumin for predicting short-term recurrence in patients with operable colorectal cancer[J]. Nutr Cancer, 2012, 64:1169-1173. DOI: 10.1080/01635581.2012.718034
[41] Han S, Li Z, Master LM, et al. Exogenous IGFBP-2 promotes proliferation, invasion, and chemoresistance to temozolomide in glioma cells via the integrin beta1-ERK pathway[J]. Br J Cancer, 2014, 111:1400-1409. DOI: 10.1038/bjc.2014.435
[42] Borg N, Guilfoyle MR, Greenberg DC, et al. Serum albumin and survival in glioblastoma multiforme[J]. J Neurooncol, 2011, 105:77-81. DOI: 10.1007/s11060-011-0562-0
[43] Schwartzbaum JA, Lal P, Evanoff W, et al. Presurgical serum albumin levels predict survival time from glioblastoma multiforme[J]. J Neurooncol, 1999, 43:35-41. DOI: 10.1023/A:1006269413998
[44] Perisanidis C, Psyrri A, Cohen EE, et al. Prognostic role of pretreatment plasma fibrinogen in patients with solid tumors: A systematic review and meta-analysis[J]. Cancer Treat Rev, 2015, 41:960-970. DOI: 10.1016/j.ctrv.2015.10.002
[45] Zhao J, Zhao M, Jin B, et al. Tumor response and survival in patients with advanced non-small-cell lung cancer: the predictive value of chemotherapy-induced changes in fibrinogen[J]. BMC Cancer, 2012, 12:330. DOI: 10.1186/1471-2407-12-330
[46] Pichler M, Hutterer GC, Stojakovic T, et al. High plasma fibrinogen level represents an independent negative prognostic factor regarding cancer-specific, metastasis-free, as well as overall survival in a European cohort of non-metastatic renal cell carcinoma patients[J]. Br J Cancer, 2013, 109:1123-1129. DOI: 10.1038/bjc.2013.443
[47] Wen J, Yang Y, Ye F, et al. The preoperative plasma fibrinogen level is an independent prognostic factor for overall survival of breast cancer patients who underwent surgical treatment[J]. Breast, 2015, 24:745-750. DOI: 10.1016/j.breast.2015.09.007
[48] Matsuda S, Takeuchi H, Kawakubo H, et al. Cumulative prognostic scores based on plasma fibrinogen and serum albumin levels in esophageal cancer patients treated with transthoracic esophagectomy: comparison with the Glasgow prognostic score[J]. Ann Surg Oncol, 2015, 22:302-310. DOI: 10.1245/s10434-014-3857-5
[49] He ZQ, Duan H, Ke C, et al. Evaluation of cumulative prognostic score based on pretreatment plasma fibrinogen and serum albumin levels in patients with newly diagnosed high-grade gliomas[J]. Oncotarget, 2017, 8:49605-49614. DOI: 10.18632/oncotarget.17849
[50] Han LH, Jia YB, Song QX, et al. Prognostic significance of preoperative lymphocyte-monocyte ratio in patients with resectable esophageal squamous cell carcinoma[J]. Asian Pac J Cancer Prev, 2015, 16:2245-2250. DOI: 10.7314/APJCP.2015.16.6.2245
[51] Guthrie GJ, Charles KA, Roxburgh CS, et al. The systemic inflammation-based neutrophil-lymphocyte ratio: experience in patients with cancer[J]. Crit Rev Oncol Hematol, 2013, 88:218-230. DOI: 10.1016/j.critrevonc.2013.03.010
[52] Zitvogel L, Tesniere A, Kroemer G. Cancer despite immunosurveillance: immunoselection and immunosubversion[J]. Nat Rev Immunol, 2006, 6:715-727. DOI: 10.1038/nri1936
[53] Inouye SK, Studenski S, Tinetti ME, et al. Geriatric syndromes: clinical, research, and policy implications of a core geriatric concept[J]. J Am Geriatr Soc, 2007, 55:780-791. DOI: 10.1111/j.1532-5415.2007.01156.x
[54] Kane RL, Shamliyan T, Talley K, et al. The association between geriatric syndromes and survival[J]. J Am Geriatr Soc, 2012, 60:896-904. DOI: 10.1111/j.1532-5415.2012.03942.x
[55] Vallet-Regi M, Manzano M, Rodriguez-Manas L, et al. Management of Cancer in the Older Age Person: An Approach to Complex Medical Decisions[J]. Oncologist, 2017, 22:335-342. DOI: 10.1634/theoncologist.2016-0276
[56] Svendsboe E, Terum T, Testad I, et al. Caregiver burden in family carers of people with dementia with Lewy bodies and Alzheimer's disease[J]. Int J Geriatr Psychiatry, 2016, 31:1075-1083. DOI: 10.1002/gps.4433
[57] Balducci L, Extermann M. Management of cancer in the older person: a practical approach[J]. Oncologist, 2000, 5:224-237. DOI: 10.1634/theoncologist.5-3-224
-
期刊类型引用(1)
1. 李贺莹,高京丕,郭鹏山,何卿豪,林蔓萍,顾硕,李景华. 铂基纳米制剂平台在医学多模态成像中的应用. 中国医学影像学杂志. 2024(01): 105-108+112 .  百度学术
百度学术
其他类型引用(0)

 作者投稿
作者投稿 专家审稿
专家审稿 编辑办公
编辑办公 邮件订阅
邮件订阅 RSS
RSS

 下载:
下载: