Difference in Gut Microbiota between the First and the Second Trimester of Pregnancy and the Association of Gut Microbiota with Gestational Diabetes Mellitus: A Prospective Cohort Study
-
摘要:
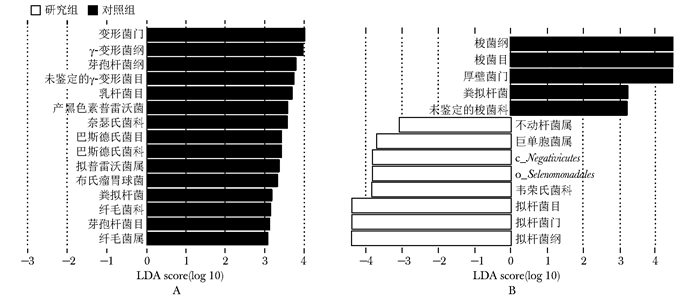
目的 探讨早/中孕期妇女的肠道菌群物种及功能特点,并分析其与妊娠期糖尿病(gestational diabetes mellitus, GDM)的关系。 方法 前瞻性收集并分析2017年5月至12月北京协和医院产科招募的早孕期孕妇的临床资料。依据孕24~28周75 g口服葡萄糖耐量试验(oral glucose tolerance test, OGTT)结果分为GDM组(研究组)和非GDM组(对照组)。分别于早孕期和中孕期收集两组孕妇粪便标本,对肠道菌群的16S rRNA V4可变区进行DNA测序及生物信息学分析。采用多因素Logistic回归分析探讨肠道菌群Alpha多样性及菌群相对丰度与GDM的关系。 结果 共145例符合纳入和排除标准的孕妇入选本研究。其中研究组34例、对照组111例。Alpha多样性分析显示,研究组早孕期Shannon指数和Simpson指数低于对照组(P均<0.05)。LEfSe分析显示,早孕期和中孕期,多个物种的相对丰度在两组间差异具有统计学意义(P均<0.05)。多因素Logistic回归分析显示,早孕期Shannon指数≤6.51(OR=3.15, 95% CI: 1.32~7.52)、Simpson指数≤0.96(OR=2.54,95% CI: 1.09~5.89)、拟普雷沃菌属(Alloprevotella)相对丰度≤0.004(OR=2.65, 95% CI: 1.09~6.44)、毛螺菌属(Lachnospira)相对丰度≤0.0107(OR=3.17, 95% CI: 1.33~7.55)是发生GDM的危险因素。肠道菌群功能预测比较显示, 早孕期时两组差异较少;中孕期时与能量代谢、糖代谢、氨基酸代谢和脂多糖(lipopolysaccharide, LPS)合成相关的通路在研究组显著富集。 结论 与健康孕妇相比,中孕期GDM患者肠道菌群的功能特点为LPS合成、能量代谢、糖代谢和氨基酸代谢相关通路显著富集; 早孕期肠道菌群物种多样性降低及某些菌属的丰度降低是发生GDM的危险因素。 Abstract:Objective To characterize the characteristics of gut microbiota and its function in the first (T1) to second trimester(T2) of pregnancy and to evaluate its association with gestational mellitus diabetes (GDM). Methods A prospective cohort study was conducted in Peking Union Medical College Hospital from May to December 2017. The pregnancies were divided into GDM group and non-GDM group (control group) according to the Results of 75 g oral glucose tolerance test at 24 to 48 weeks of gestation. Stool samples of all participants were collected in the first and the second trimester. The V4 region of the 16S rRNA gene was sequenced and analyzed. Multivariate Logistic regression analysis was used to investigate the relationship between Alpha diversity, relative abundance of intestinal flora and GDM. Results A total of 145 pregnancies, of whom 34 diagnosed with GDM (GDM group) and 111 healthy (control group) were analyzed. The Alpha diversity of the GDM group (Shannon index and Simpson index) was significantly lower than that of the control group (P < 0.05). LEfSe analysis revealed that the relative abundance of several genera was different between the 2 groups in T1 or T2. Multivariate Logistic analysis showed that Shannon index ≤6.51 (OR=3.15, 95% CI: 1.32-7.52), Simpson index ≤0.96 (OR=2.54, 95% CI: 1.09-5.89), the lower relative abundance of Alloprevotella(OR=2.65, 95% CI: 1.09-6.44) and Lachnospira(OR=3.17, 95% CI: 1.33-7.55) in the first trimester were risk factors for GDM. The pathways of LPS biosynthesis, energy metabolism, glucose metabolism and amino acid metabolism of gut microbiome revealed through the Tax4Fun analysis were significantly enriched in the GDM group in T2. Conclusions Compared with healthy controls, the functional characteristics of intestinal microflora in GDM patients during the second trimester were significantly enriched in functional pathways related to LPS synthesis, energy metabolism, glucose metabolism and amino acid metabolism. The decreases of the diversity as well as the relative abundance of some genus in the early pregnancy are the risk factors for GDM. -
Key words:
- gestational diabetes mellitus /
- gut microbiota /
- abundance /
- diversity
作者贡献:王佩负责研究设计、实施、数据采集、统计分析、撰写论文;马良坤指导研究设计;刘俊涛参与研究设计和实施、论文修改、经费支持。利益冲突:无 -
表 1 两组孕妇的临床特征比较
指标 研究组(n=34) 对照组(n=111) P值 年龄(x±s,岁) 35.5±4.3 32.3±3.9 <0.001 经产妇[n(%)] 13(38.2) 24(21.6) 0.052 孕前BMI(x±s,kg/m2) 22.8±3.8 21.9±2.6 0.187 75 g OGTT(x±s,mmol/L) 0 h血糖 4.9±0.4 4.5±0.2 <0.001 1 h血糖 9.2±1.6 7.3±1.3 <0.001 2 h血糖 8.3±1.3 6.4±0.9 <0.001 GDM诊断孕周[M(P25, P75),周] 24.9(24.3,25.6) 24.7(24.1,25.4) 0.153 早孕期留取标本孕周[M(P25, P75),周] 12.6(12.0,13.6) 12.7(12.1,13.4) 0.632 中孕期留取标本孕周[M(P25, P75),周] 25.5(24.6,26.4) 25.5(24.4,26.7) 0.647 BMI: 体质量指数;OGTT: 口服葡萄糖耐量试验;GDM: 妊娠期糖尿病 表 2 两组早孕期肠道菌群Alpha多样性比较及多因素Logistic回归分析
Alpha多样性指数 研究组(n=34) 对照组(n=111) P值 多因素Logistic回归分析* 取值范围 OR(95% CI) P值 Chao1指数[M(P25, P75)] 918.9(749.4, 1450.7) 1082.3(857.1, 2037.1) 0.119 ≤1544.1 1 >1544.1 0.49(0.19~1.27) 0.144 Shannon指数(x±s) 6.19±0.93 6.60±0.84 0.019 ≤6.51 3.15(1.32~7.52) 0.009 >6.51 1 Simpson指数[M(P25, P75)] 0.96(0.94, 0.97) 0.97(0.95, 0.98) 0.004 ≤0.96 2.54(1.09~5.89) 0.030 >0.96 1 *多因素Logistic回归分析调整因素包括年龄和孕前体质量指数 表 3 早孕期肠道菌群主要物种与GDM关系的多因素Logistic回归分析结果
-
[1] Committee on Practice Bulletins-Obstetrics. ACOG Practice Bulletin No. 190: Gestational Diabetes Mellitus[J]. Obstet Gynecol, 2018, 131: e49-e64. doi: 10.1097/AOG.0000000000002501 [2] Gao C, Sun X, Lu L, et al. Prevalence of gestational diabetes mellitus in mainland China: A systematic review and meta-analysis[J]. J Diabetes Investig, 2019, 10: 154-162. doi: 10.1111/jdi.12854 [3] Johns EC, Denison FC, Norman JE, et al. Gestational Diabetes Mellitus: Mechanisms, Treatment, and Complications[J]. Trends Endocrinol Metab, 2018, 29: 743-754. doi: 10.1016/j.tem.2018.09.004 [4] Kim C, Newton KM, Knopp RH. Gestational diabetes and the incidence of type 2 diabetes: a systematic review[J]. Diabetes Care, 2002, 25: 1862-1868. doi: 10.2337/diacare.25.10.1862 [5] Boney CM, Verma A, Tucker R, et al. Metabolic syndrome in childhood: association with birth weight, maternal obesity, and gestational diabetes mellitus[J]. Pediatrics, 2005, 115: e290-e296. doi: 10.1542/peds.2004-1808 [6] Plows JF, Stanley JL, Baker PN, et al. The Pathophysiology of Gestational Diabetes Mellitus[J]. Int J Mol Sci, 2018, 19: 3342. doi: 10.3390/ijms19113342 [7] Qin J, Li Y, Cai Z, et al. A metagenome-wide association study of gut microbiota in type 2 diabetes[J]. Nature, 2012, 490: 55-60. doi: 10.1038/nature11450 [8] Cani PD, Osto M, Geurts L, et al. Involvement of gut microbiota in the development of low-grade inflammation and type 2 diabetes associated with obesity[J]. Gut Microbes, 2012, 3: 279-288. doi: 10.4161/gmic.19625 [9] 焦禹豪, 张奉春. 肠道菌群与人体免疫系统相关性研究方兴未艾[J]. 协和医学杂志, 2019, 10: 193-196. doi: 10.3969/j.issn.1674-9081.2019.03.001 Jiao YH, Zhang FC. New Insights into Research on the Role of Gut Microbiota in Human Immune System[J]. Xiehe Yixue Zazhi, 2019, 10: 193-196. doi: 10.3969/j.issn.1674-9081.2019.03.001 [10] Crusell MKW, Hansen TH, Nielsen T, et al. Gestational diabetes is associated with change in the gut microbiota composition in third trimester of pregnancy and postpartum[J]. Microbiome, 2018, 6: 89. doi: 10.1186/s40168-018-0472-x [11] Ferrocino I, Ponzo V, Gambino R, et al. Changes in the gut microbiota composition during pregnancy in patients with gestational diabetes mellitus (GDM)[J]. Sci Rep, 2018, 8: 12216. doi: 10.1038/s41598-018-30735-9 [12] 刘誉, 马京梅, 秦胜堂, 等. 妊娠期糖尿病患者治疗前后肠道菌群变化及其与血糖的相关性[J]. 中华围产医学杂志, 2020, 23: 98-104. doi: 10.3760/cma.j.issn.1007-9408.2020.02.005 Liu Y, Ma JM, Qin ST, et al. Different characteristics of gut microbiota before and after management of women with gestational diabetes mellitus and the association with blood glucose level[J]. Zhonghua Weichan Yixue Zazhi, 2020, 23: 98-104. doi: 10.3760/cma.j.issn.1007-9408.2020.02.005 [13] Kuang YS, Lu JH, Li SH, et al. Connections between the human gut microbiome and gestational diabetes mellitus[J]. GigaScience, 2017, 6: 1-12. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC5597849/pdf/gix058.pdf [14] 中华医学会妇产科学分会产科学组, 中华医学会围产医学分会妊娠合并糖尿病协作组. 妊娠合并糖尿病诊治指南(2014)[J]. 中华妇产科杂志, 2014, 49: 561-569. https://www.cnki.com.cn/Article/CJFDTOTAL-TNBL201411002.htm Obstetrics group of Obstetrics and Gynecology branch of Chinese Medical Association, Chinese Medical Association perinatal medicine branch, gestational diabetes cooperation group. Guidelines for the diagnosis and treatment of gestational diabetes mellitus (2014)[J]. Zhonghua Fuchanke Zazhi, 2014, 49: 56-569. https://www.cnki.com.cn/Article/CJFDTOTAL-TNBL201411002.htm [15] Chen CC, Wu WK, Chang CM, et al. Comparison of DNA stabilizers and storage conditions on preserving fecal microbiota profiles[J]. J Formos Med Assoc, 2020, 119: 1791-1798. doi: 10.1016/j.jfma.2020.01.013 [16] Aβhauer KP, Wemheuer B, Daniel R, et al. Tax4Fun: predicting functional profiles from metagenomic 16S rRNA data[J]. Bioinformatics, 2015, 31: 2882-2884. doi: 10.1093/bioinformatics/btv287 [17] Koren O, Goodrich JK, Cullender TC, et al. Host remodeling of the gut microbiome and metabolic changes during pregnancy[J]. Cell, 2012, 150: 470-480. doi: 10.1016/j.cell.2012.07.008 [18] Lloyd-Price J, Abu-Ali G, Huttenhower C. The healthy human microbiome[J]. Genome Med, 2016, 8: 51. doi: 10.1186/s13073-016-0307-y [19] Le Chatelier E, Nielsen T, Qin J, et al. Richness of human gut microbiome correlates with metabolic markers[J]. Nature, 2013, 500: 541-546. doi: 10.1038/nature12506 [20] Ma S, You Y, Huang L, et al. Alterations in Gut Microbiota of Gestational Diabetes Patients During the First Trimester of Pregnancy[J]. Front Cell Infect Microbiol, 2020, 10: 58. doi: 10.3389/fcimb.2020.00058 [21] DiGiulio DB, Callahan BJ, McMurdie PJ, et al. Temporal and spatial variation of the human microbiota during pregnancy[J]. Proc Natl Acad Sci U S A, 2015, 112: 11060-11065. doi: 10.1073/pnas.1502875112 [22] Taddei CR, Cortez RV, Mattar R, et al. Microbiome in normal and pathological pregnancies: A literature overview[J]. Am J Reprod Immunol, 2018, 80: e12993. doi: 10.1111/aji.12993 [23] Fugmann M, Breier M, Rottenkolber M, et al. The stool microbiota of insulin resistant women with recent gestational diabetes, a high risk group for type 2 diabetes[J]. Sci Rep, 2015, 5: 13212. doi: 10.1038/srep13212 [24] Liu Z, Li J, Liu H, et al. The intestinal microbiota associated with cardiac valve calcification differs from that of coronary artery disease[J]. Atherosclerosis, 2019, 284: 121-128. doi: 10.1016/j.atherosclerosis.2018.11.038 [25] Kong C, Gao R, Yan X, et al. Probiotics improve gut microbiota dysbiosis in obese mice fed a high-fat or high-sucrose diet[J]. Nutrition, 2019, 60: 175-184. doi: 10.1016/j.nut.2018.10.002 [26] Kelly TN, Bazzano LA, Ajami NJ, et al. Gut Microbiome Associates With Lifetime Cardiovascular Disease Risk Profile Among Bogalusa Heart Study Participants[J]. Circ Res, 2016, 119: 956-964. doi: 10.1161/CIRCRESAHA.116.309219 [27] Bryant MP, Small N. Characteristics of two new genera of anaerobic curved rods isolated from the rumen of cattle[J]. J Bacteriol, 1956, 72: 22-26. doi: 10.1128/jb.72.1.22-26.1956 [28] Zhang Q, Xiao X, Li M, et al. Vildagliptin increases butyrate-producing bacteria in the gut of diabetic rats[J]. PLoS One, 2017, 12: e0184735. doi: 10.1371/journal.pone.0184735 [29] Leonel AJ, Alvarez-Leite JI. Butyrate: implications for intestinal function[J]. Curr Opin Clin Nutr Metab Care, 2012, 15: 474-479. doi: 10.1097/MCO.0b013e32835665fa [30] Cani PD, Amar J, Iglesias MA, et al. Metabolic endotoxe-mia initiates obesity and insulin resistance[J]. Diabetes, 2007, 56: 1761-1772. doi: 10.2337/db06-1491 [31] Ploger S, Stumpff F, Penner GB, et al. Microbial butyrate and its role for barrier function in the gastrointestinal tract[J]. Ann N Y Acad Sci, 2012, 1258: 52-59. doi: 10.1111/j.1749-6632.2012.06553.x [32] Zheng W, Xu Q, Huang W, et al. Gestational Diabetes Mellitus Is Associated with Reduced Dynamics of Gut Microbiota during the First Half of Pregnancy[J]. mSystems, 2020, 5: e00109-e00120. http://www.researchgate.net/publication/340148277_Gestational_Diabetes_Mellitus_Is_Associated_with_Reduced_Dynamics_of_Gut_Microbiota_during_the_First_Half_of_Pregnancy/download?ivk_sa=1024320u [33] Callaway LK, McIntyre HD, Barrett HL, et al. Probiotics for the Prevention of Gestational Diabetes Mellitus in Overweight and Obese Women: Findings From the SPRING Double-Blind Randomized Controlled Trial[J]. Diabetes Care, 2019, 42: 364-371. http://www.researchgate.net/publication/330498522_Probiotics_for_the_Prevention_of_Gestational_Diabetes_Mellitus_in_Overweight_and_Obese_Women_Findings_From_the_SPRING_Double-Blind_Randomized_Controlled_Trial [34] Zhang J, Ma S, Wu S, et al. Effects of Probiotic Supplement in Pregnant Women with Gestational Diabetes Mellitus: A Systematic Review and Meta-Analysis of Randomized Controlled Trials[J]. J Diabetes Res, 2019, 2019: 5364730. http://www.ncbi.nlm.nih.gov/pubmed/31583250 -


 作者投稿
作者投稿 专家审稿
专家审稿 编辑办公
编辑办公 邮件订阅
邮件订阅 RSS
RSS


 下载:
下载: