Relationship between HbA1c and the Time in Range Derived from Flash Glucose Monitoring System
-
摘要:
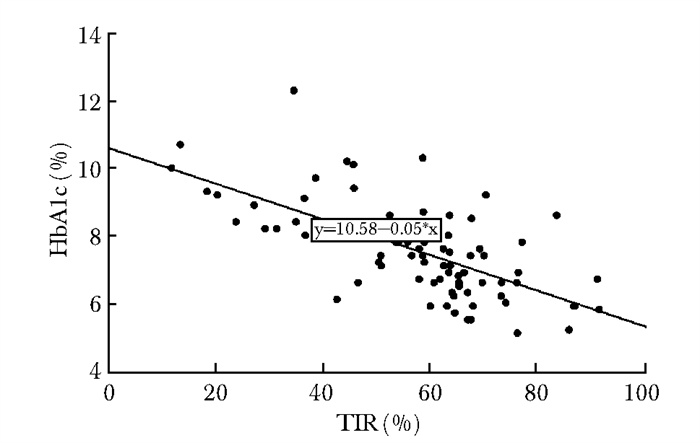
目的 分析中国成人1型糖尿病(type 1 diabetes mellitus, T1DM)患者扫描式葡萄糖监测系统(flash glucose monitoring system, FGMS)衍生的目标范围时间(time in range, TIR)与糖化血红蛋白(glycated hemoglobin, HbA1c)的关系。 方法 前瞻性收集并分析2018年10月至2019年3月北京协和医院内分泌科门诊招募的成人T1DM患者的临床资料。患者均测定HbA1c,并佩戴医院版FGMS 14 d,计算TIR以及葡萄糖变异系数(coefficient of variation, CV)等指标。采用Spearman法分析TIR与HbA1c的相关性,采用简单线性回归法分析TIR与HbA1c的关系。 结果 共77例符合纳入和排除标准的T1DM患者纳入分析,HbA1c为(7.5±1.3)%,TIR为62.0(48.7,67.8)%,CV为(39.7± 8.1)%。Spearman相关性分析显示,HbA1c与TIR呈负相关(r=-0.645,P<0.001);线性回归方程为:HbA1c=10.58-0.05×TIR,TIR每增加10%,HbA1c下降0.5%。分层分析结果显示,血糖稳定(CV<36%)/血糖不稳定(CV≥36%)患者的HbA1c与TIR均呈负相关(r=-0.774,P<0.001;r=-0.560,P<0.001),且在血糖稳定的患者中二者相关性更强。对于同一TIR,血糖稳定者的HbA1c较血糖不稳定者更高。 结论 在中国成人T1DM患者中,FGMS衍生的TIR与HbA1c呈负相关,可用于指导血糖管理,但TIR与HbA1c的相关性可能受血糖变异性影响。 -
关键词:
- 1型糖尿病 /
- 扫描式葡萄糖监测系统 /
- 目标范围时间
Abstract:Objective To explore the relationship between HbA1c and time in range (TIR) derived from flash glucose monitoring system (FGMS) in Chinese adults with type 1 diabetes mellitus (T1DM). Methods Adult T1DM patients attended the outpatient department of Peking Union Medical College Hospital (PUMCH) from October 2018 to March 2019 were included. HbA1c and data of FGMS were obtained at the same time. TIR was calculated, and the relationship between TIR and HbA1c was investigated by Spearman correlation and regression analysis. Results A total of 77 patients who met the inclusion and exclusion criteria were included in the analysis. The average HbA1c was (7.5±1.3)%; TIR was 62.0 (48.7, 67.8)% and coefficient of variation(CV) was (39.7±8.1)%. TIR derived from FGMS had a negative liner correlation with HbA1c (r=-0.645, P < 0.001). The regression equation is: HbA1c=10.58-0.05×TIR. The HbA1c level is decreased by 0.5% for every 10% increase in TIR. TIR was negatively correlated with HbA1c in patients with both stable glucose (CV < 36%) and unstable glucose (CV≥36%), but the correlation coefficient between TIR and HbA1c in patients with stable glucose was higher. For a specific TIR, HbA1c was higher in patients with stable glucose. Conclusion The FGMS-derived TIR could be helpful in the glucose management in Chinese adults with T1DM, and glucose variability should be taken into consideration while interpreting the relationship between TIR and HbA1c. -
Key words:
- type 1 diabetes mellitus /
- flash glucose monitoring system /
- time in range
作者贡献:邓明群负责数据整理、统计学分析、撰写论文;周丽媛、翟笑、刘洁颖、付俊玲、虞睿琪、潘妘頔、马丽媛负责患者病史的采集、体格检查、血样采集、FGMS佩戴等;于淼、许建萍、李文慧、冯凯负责患者的招募与纳入;肖新华负责研究设计、论文修订。利益冲突:无 -
图 2 血糖稳定/不稳定患者HbA1c与TIR散点图
HbA1c、TIR: 同图 1
表 1 血糖稳定/不稳定患者TIR对应的HbA1c
TIR(%) HbA1c(%) 所有患者 CV<36% CV≥36% 0.0 10.6 11.0 10.5 10.0 10.1 10.5 10.0 20.0 9.5 10.0 9.4 30.0 9.0 9.5 8.8 40.0 8.5 8.9 8.3 50.0 8.0 8.4 7.7 60.0 7.4 7.9 7.2 70.0 6.9 7.4 6.6 80.0 6.4 6.8 6.1 90.0 5.8 6.3 5.5 100.0 5.3 5.8 5.0 HbA1c、TIR:同图 1;CV: 变异系数 -
[1] Beck RW, Connor CG, Mullen DM, et al. The Fallacy of Average: How Using HbA1c Alone to Assess Glycemic Control Can Be Misleading[J]. Diabetes Care, 2017, 40: 994-999. doi: 10.2337/dc17-0636 [2] Danne T, Revital N, Tadej B, et al. International Consensus on Use of Continuous Glucose Monitoring[J]. Diabetes Care, 2017, 40: 1631-1640. doi: 10.2337/dc17-1600 [3] Lu JY, Ma XJ, Zhou J, et al. Association of Time in Range, as Assessed by Continuous Glucose Monitoring, With Diabetic Retinopathy in Type 2 Diabetes[J]. Diabetes Care, 2018, 41: 2370-2376. doi: 10.2337/dc18-1131 [4] American Diabetes Association. Disclosures: Standards of Medical Care in Diabetes—2020[J]. Diabetes Care, 2020, 43: S205-S206. doi: 10.2337/dc20-Sdis [5] 中华医学会糖尿病学分会. 中国持续葡萄糖监测临床应用指南(2017年版)[J]. 中华糖尿病杂志, 2017, 9: 667-675. doi: 10.3760/cma.j.issn.1674-5809.2017.11.002 [6] Beck RW, Tonya RW, Katrina R, et al. Effect of Continu-ous Glucose Monitoring on Glycemic Control in Adults With Type 1 Diabetes Using Insulin Injections: The DIAMOND Randomized Clinical Trial[J]. JAMA, 2017, 317: 371-378. doi: 10.1001/jama.2016.19975 [7] Ruedy KJ, Tamborlane WV. The Landmark JDRF Continu-ous Glucose Monitoring Randomized Trials: a Look Back at the Accumulated Evidence[J]. J Cardiovasc Transl Res, 2012, 5: 380-387. doi: 10.1007/s12265-012-9364-9 [8] Ólafsdóttir AF, William P, Jan B, et al. A Randomized Clinical Trial of the Effect of Continuous Glucose Monitoring on Nocturnal Hypoglycemia, Daytime Hypoglycemia, Glycemic Variability, and Hypoglycemia Confidence in Persons with Type 1 Diabetes Treated with Multiple Daily Insulin Injections (GOLD-3)[J]. Diabetes Technol Ther, 2018, 20: 274-284. doi: 10.1089/dia.2017.0363 [9] Battelino T, Conget I, Olsen B, et al. The use and efficacy of continuous glucose monitoring in type 1 diabetes treated with insulin pump therapy: a randomised controlled trial[J]. Diabetologia, 2012, 55: 3155-3162. doi: 10.1007/s00125-012-2708-9 [10] Ajjan RA. How Can We Realize the Clinical Benefits of Continuous Glucose Monitoring? [J]. Diabetes Technol Ther, 2017, 19: 27-36. [11] Tanenbaum ML, Adams RN, Lanning MS, et al. Using Cluster Analysis to Understand Clinician Readiness to Promote Continuous Glucose Monitoring Adoption[J]. J Diabetes Sci Technol, 2018, 12: 1108-1115. doi: 10.1177/1932296818786486 [12] 中华医学会糖尿病学分会血糖监测学组. 中国扫描式葡萄糖监测技术临床应用专家共识[J]. 中华糖尿病杂志, 2018, 10: 697-700. [13] Angellotti E, Sangeetha M, Siegel RD, et al. The Calculation of the Glucose Management Indicator Is Influenced by the Continuous Glucose Monitoring System and Patient Race[J]. Diabetes Technol Ther, 2020, 22: 651-657. doi: 10.1089/dia.2019.0405 [14] Beck RW, Bergenstal RM, Riddlesworth TD, et al. Validation of Time in Range as an Outcome Measure for Diabetes Clinical Trials[J]. Diabetes Care, 2019, 42: 400-405. doi: 10.2337/dc18-1444 [15] Beck RW, Bergenstal RM, Cheng PY, et al. The Relationships Between Time in Range, Hyperglycemia Metrics, and HbA1c[J]. J Diabetes Sci Technol, 2019, 13: 614-626. doi: 10.1177/1932296818822496 [16] Vigersky RA, Chantal M. The Relationship of Hemoglobin A1C to Time-in-Range in Patients with Diabetes[J]. Diabetes Technol Ther, 2019, 2: 81-85. [17] American Diabetes Association. Diabetes Technology: Stan-dards of Medical Care in Diabetes—2020[J]. Diabetes Care, 2020, 43: S77-S88. doi: 10.2337/dc20-S007 [18] Lu J, Ma X, Zhang L, et al. Glycemic variability modifies the relationship between time in range and hemoglobin A1c estimated from continuous glucose monitoring: A preliminary study[J]. Diabetes Res Clin Pract, 2020, 161: 108032. doi: 10.1016/j.diabres.2020.108032 -


 作者投稿
作者投稿 专家审稿
专家审稿 编辑办公
编辑办公 邮件订阅
邮件订阅 RSS
RSS


 下载:
下载: